外科病理学实践:诊断过程的初学者指南 | 第21章 淋巴结
第21章 淋巴结(Lymph Node)
正常组织学(Normal Histology)
The normal or benign lymph node is composed of a collection of follicles and interfollicular areas surrounded by sinuses (spaces mostly filled with histiocytes), vessels, and sometimes fat. Lymph flows from the subcapsular sinuses, through the medullary sinuses in the lymph node, and out the hilum. The follicles represent areas of maturing B cells (CD20+), whereas the interfollicular areas are mostly mature T cells (CD3+).
正常或良性淋巴结由滤泡区和滤泡间区组成,周围有被膜下窦(主要充满组织细胞)、血管,有时还有脂肪。淋巴从被膜下窦流出,经淋巴结内的髓窦流出门部。滤泡代表成熟的B细胞(CD20+),而滤泡间区域主要是成熟的T细胞(CD3+)。
Follicles begin as primary follicles, or aggregates of antigen-naïve B cells. As they mature into secondary follicles they acquire germinal centers, which are visible as targetoid nodules within the follicles (Figure 21.1). The dark outer rim of the follicle is the displaced remains of the primary follicle and is called the mantle zone, still composed of antigen-naïve B cells. Once exposed to antigen, the B cells move to the germinal center and become centroblasts, large cells with primitive-looking nuclei. From there they either mature into centrocytes or die through apoptosis. Finally, B cells leave the germinal center genetically altered to circulate as memory B cells, which may ultimately differentiate into plasma cells if they meet their antigen.
滤泡最初是初级滤泡,或未接触抗原的B细胞(译注:童贞B细胞)的聚集灶。当它们成熟为次级滤泡时,形成生发中心,表现为滤泡内的靶环样结节(图21.1)。滤泡最外层的深染边缘是初级滤泡移位留下的残余物,称为套区,仍然是童贞B细胞。一旦接触抗原,B细胞移动到生发中心并成为成中心母细胞,即看似原始细胞核的大细胞。从那里,它们要么成熟为中心细胞,要么死于凋亡。最后,B细胞离开生发中心,经过基因改造,成为记忆B细胞并进入血液循环,如果遇到抗原,记忆B细胞最终可能分化为浆细胞。
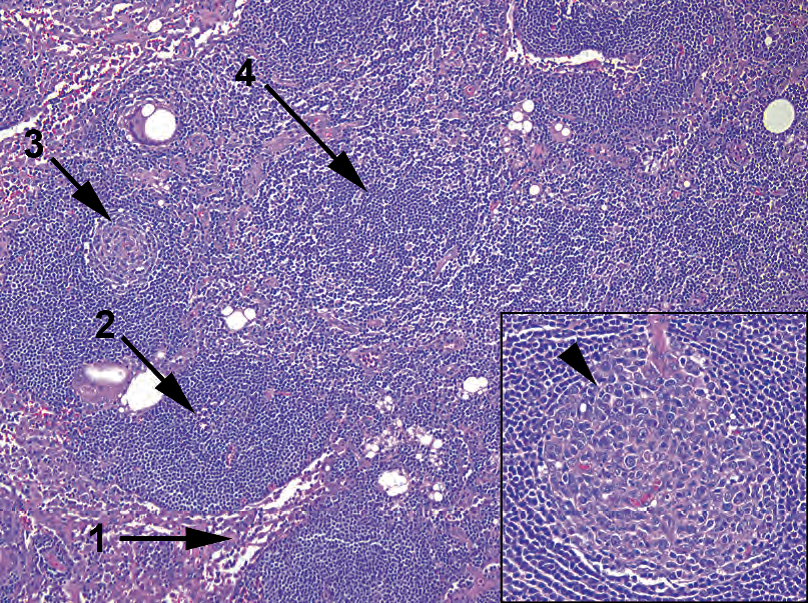
Figure 21.1. Normal lymph node. The sinuses are visible mainly as loose collections of histiocytes (1). Primary follicles (2) are collections of B cells lacking germinal centers. Secondary follicles contain germinal centers (3). The space between the follicles, or paracortex (4), is composed of T cells and shows a characteristic spotted or mottled appearance. Inset: A normal germinal center should be polarized, with large centroblasts clustered at one side of the follicle (arrowhead), creating a lopsided appearance.
图21.1 正常淋巴结。淋巴窦主要是松散的组织细胞聚集(1)。初级滤泡(2)是缺乏生发中心的B细胞聚集。次级滤泡含有生发中心(3)。滤泡之间的区域,或副皮质区(4),由T细胞组成,并显示特征性斑点样或斑驳样外观。插图:正常的生发中心应该有极性,大的中心母细胞聚集在滤泡的一侧(箭头),形成不平衡的外观。
Other normal germinal center components include the supporting follicular dendritic cells and tingible body macrophages, which clean up the apoptotic debris. These appear as relatively clear cells within the germinal center, with visible “dust specks” in the cytoplasm (Figure 21.2). Germinal centers may be found in any hotbed of lymphocyte activity outside the lymph nodes, but the morphology and staining pattern are preserved.
正常生发中心的其他成分包括支持性滤泡树突状细胞和可染小体巨噬细胞,后者清除凋亡碎屑。这些细胞在生发中心内表现为相对透明的细胞,细胞质可见“尘埃斑点”(图21.2)。在淋巴结外的任何淋巴细胞活动的温床中都可以发现生发中心,但其形态和染色模式得以保留。
The paracortex, or interfollicular area, may occupy most of the lymph node in some cases. This absence of obvious follicles is not necessarily a reason for concern. The benign paracortex should have a mottled appearance due to the scattered pale histiocytes among the T cells.
在某些情况下,副皮质区或滤泡间区可能占据大部分淋巴结。缺乏明显的滤泡不一定值得关注。良性副皮质应当呈现斑驳的外观,因为在T细胞之间散在分布的淡染的组织细胞。

Figure 21.2. Germinal center. Other components of a benign germinal center include tingible body macrophages (circle) and large centroblasts with prominent nucleoli (arrow). The germinal center is surrounded by the mature B cells of the mantle zone (arrowhead).
图21.2 生发中心。良性生发中心的其他成分包括可染小染巨噬细胞(圆圈)和核仁显著的大中心母细胞(箭)。生发中心围绕着套区的成熟B细胞(箭头)。
淋巴瘤概念(Lymphoma, Conceptually)
The word lymphoma means a malignancy of the lymphoid system and usually implies a solid tumor mass. However, remember that many of the lymphomas can have an associated leukemia, which is when the neoplastic cells invade the bone marrow and become circulating (Table 21.1). Among the myeloid leukemias, discussed in Chapter 20, solid tumor disease is uncommon but exists (such as the chloroma, or granulocytic sarcoma).
淋巴瘤是淋巴系统的恶性肿瘤,通常指实体肿瘤。然而,许多淋巴瘤可能伴有白血病,即肿瘤细胞侵入骨髓并进入血液循环(表21.1)。在第20章讨论的髓系白血病中,实体瘤疾病并少见,但确实存在(如,绿色瘤或粒细胞肉瘤)。
Table 21.1. Lymphomas and associated leukemias.
表21.1 淋巴瘤和相关白血病。
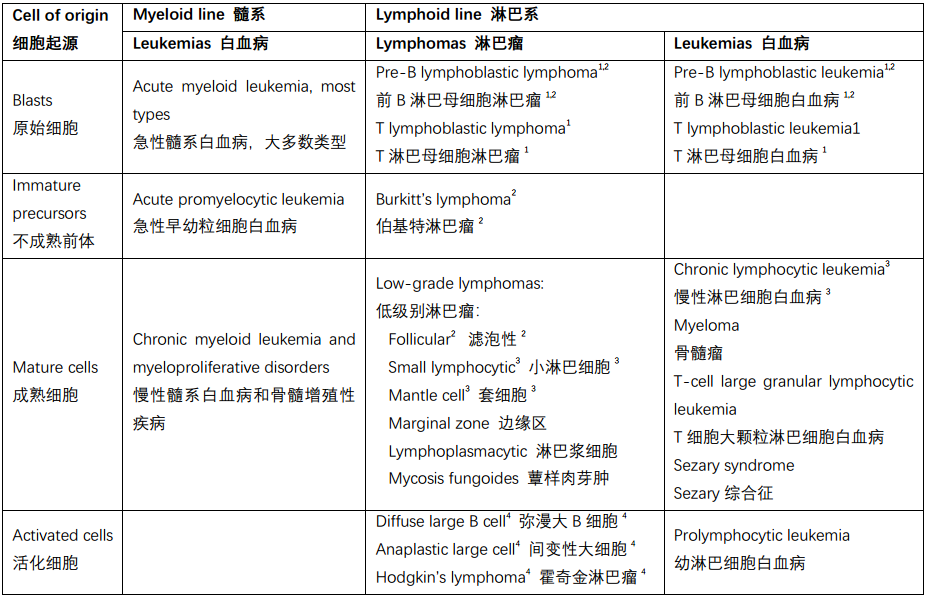
Markers go in batches: 1TdT, CD34+; 2CD10+; 3CD5+; 4CD30+.
分批进行标记:1TdT,CD34+;2CD10+;3CD5+;4CD30+。
This chapter covers several major categories of lymphomas:
本章涵盖了几大类淋巴瘤:
Lymphoblastic (neoplasms of precursor cells, or lymphoblasts): These cells resemble myeloblasts and are the solid tumor counterpart to the acute lymphoblastic leukemias.
淋巴母细胞(前体细胞或淋巴母细胞的肿瘤):这些细胞类似于原粒细胞,是急性淋巴母细胞白血病对应的实体瘤。
Low-grade B cell lymphomas (neoplasms of mature B cells): Like the chronic leukemias, these are indolent and simmering and are diseases of adults. They have a low mitotic rate and are therefore not susceptible to most chemotherapy.
低级别B细胞淋巴瘤(成熟B细胞的肿瘤):与慢性白血病一样,是惰性、慢性、成人疾病。低核分裂率,对大多数化疗不敏感。
High-grade (aggressive) lymphomas (neoplasms of activated B cells and T cells [activated means exposed to the target antigen] or that resemble activated cells): These have a high mitotic rate but are therefore potentially curable through chemotherapy.
高级别(侵袭性)淋巴瘤(活化B细胞和T细胞的肿瘤[活化意味着暴露于目标抗原]或类似活化细胞的肿瘤):高核分裂率,化疗可能治愈。
Hodgkin’s lymphomas: As a group, these are neoplasms in which the neoplastic cells are a minority population, with a variable mixed inflammatory background. The prototypical tumor cell is the Reed-Sternberg cell, of which there are many variants.
霍奇金淋巴瘤:作为一组肿瘤,肿瘤细胞群只占少数,具有不同程度的混合性炎症背景。原型肿瘤细胞是RS细胞,它有许多变体。
Plasmacytoma: Plasmacytomas are neoplasms of plasma cells
浆细胞瘤:是浆细胞的肿瘤
Other: Other lymphomas include T-cell neoplasms and non-B, non-T cell types.
其他:其他淋巴瘤包括T细胞肿瘤、非B非T细胞类型。
Many of the lymphomas can be placed into categories by nuclear morphology, and learning to recognize the “look” of each group is important. The lymphoblastic lymphomas have immature chromatin, which means the texture is very fine grained, with small nucleoli and an indistinct nuclear membrane, much like the myeloblasts in acute myeloid leukemia. On H&E stain, they may be mistaken for small cell carcinoma. The low-grade neoplasms resemble normal lymphocytes, with small condensed nuclei. The high-grade lymphomas show very carcinoma-like nuclei: they are large (compared with lymphocytes) and pleomorphic, with prominent nucleoli and coarse nuclear membranes. Hodgkin’s lymphomas are the hardest to identify, usually, as the diagnostic cells (Reed-Sternberg cells and variants) may be few and far between. However, they do resemble the high-grade lymphoma nuclei in terms of the chromatin pattern.
许多淋巴瘤可以根据细胞核形态进行分类,学会识别每组的“外观”很重要。淋巴母细胞淋巴瘤有不成熟的染色质,这意味着其质地非常细腻颗粒状,有小核仁,核膜不清晰,很像急性髓系白血病中的原粒细胞。HE染色可能误认为小细胞癌。低级别肿瘤类似于正常淋巴细胞,核小而凝缩。高级别淋巴瘤的核很像癌:大(与淋巴细胞相比),多形性,核仁显著,核膜粗糙。霍奇金淋巴瘤通常最难识别,因为诊断细胞(RS细胞和变体)可能很少,非常稀疏。然而,就染色质模式而言,它们确实很像高级淋巴瘤细胞核。
Recognizing a lymphoma in an extranodal site, especially a tumor of unknown origin, takes practice. Clues to lymphoma include a relatively homogeneous, sheet-like growth of malignant cells; a lack of cell-to-cell cohesiveness or architecture; nuclei that are highly irregular in shape or contour; and an accentuation of cell density around vessels (especially in the central nervous system; Figure 21.3). Most should stain for CD45, the common leukocyte antigen, or for specific B or T markers. Positive staining for melanoma markers or cytokeratins rules out lymphoma. Sarcoma markers should be used with caution, though, as many of the familiar stains (CD117, CD34, etc.) also stain hematopoietic elements.
识别结外部位的淋巴瘤,尤其是来源不明的肿瘤,需要一些实践经验。淋巴瘤的线索包括恶性细胞相对均匀的片状生长;缺乏细胞间的粘附性或结构;核形状或轮廓高度不规则;血管周围的细胞密度增强(尤其是中枢神经系统;图21.3)。大多数淋巴瘤呈CD45阳性(CD45是白细胞共同抗原,LCA),或表达特定的B或T标记物。表达黑色素瘤标记物或CK则排除淋巴瘤。但肉瘤标记物应谨慎使用,因为许多常见的抗体(CD117、CD34,等)也表达于造血成分。
弥漫大B细胞淋巴瘤(Diffuse large B-cell lymphoma)
As the most common lymphoma, you will see diffuse large B-cell lymphoma (DLBCL) frequently. DLBCL is essentially a final common pathway in lymphoma; although it can arise spontaneously, it can also arise from the setting of any other low-grade B-cell lymphoma or from Hodgkin’s lymphoma. The “diffuse” is used here as an opposite of follicular or nodular, and it implies sheet-like growth. The “large” should be interpreted with caution—what is large in hematopathology may still be fairly small next to a squamous cell.
作为最常见的淋巴瘤,你会经常看到弥漫大B细胞淋巴瘤(DLBCL)。DLBCL本质上是淋巴瘤的最终共同途径;虽然它可以自发产生,但也可以由任何其他低级别B细胞淋巴瘤或霍奇金淋巴瘤进展而来。“弥漫性”一词是相对于滤泡或结节而言,它意味着成片生长。“大”的判读应谨慎,血液病理学中的大细胞可能仍然比相邻鳞状细胞小很多。
(译注:核大于或等于组织细胞核,或者大于小淋巴细胞核的2倍)
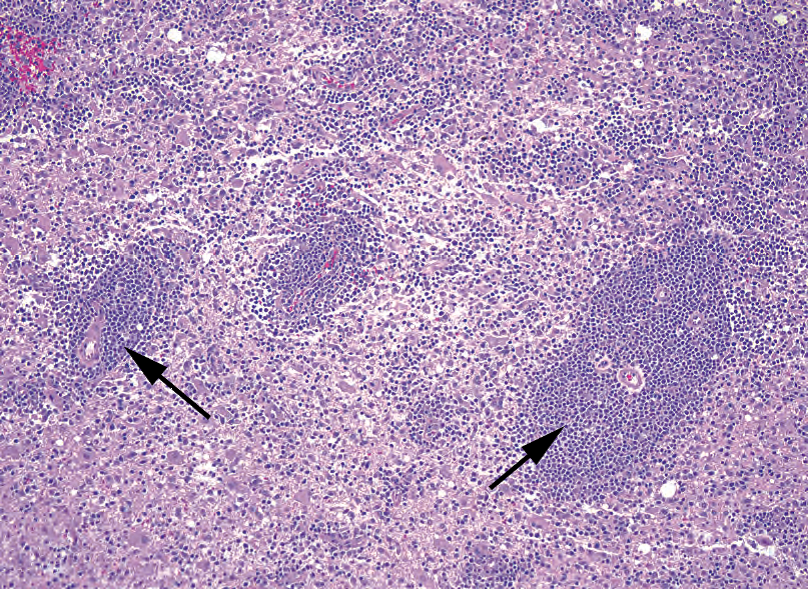
Figure 21.3. Diffuse large B-cell lymphoma in the central nervous system. The tendency of the malignant cells to cluster around blood vessels (arrows) is typical of lymphoma within the brain.
图21.3 中枢神经系统弥漫大B细胞淋巴瘤。恶性细胞往往聚集在血管周围(箭),是脑内淋巴瘤的典型特征。

Figure 21.4. Diffuse large B-cell lymphoma. The usual appearance is that of sheets of discohesive cells that do not form any recognizable architectural patterns (such as glands or trabeculae). The cells typically have large nuclei, irregular and prominent nuclear membranes, and nucleoli (arrow). Compare the cell size to a background lymphocyte (arrowhead).
图21.4 弥漫大B细胞淋巴瘤。通常表现为成片的不粘附细胞,不形成任何可识别的结构模式(如腺体或小梁)。细胞常有大核,核膜明显且不规则,并有核仁(箭)。将细胞大小与背景淋巴细胞(箭头)进行比较。
Diffuse large B-cell lymphoma is not usually mistaken for a benign entity; the nuclei are too abnormal. However, it may be mistaken for other types of malignancy, especially given its tendency to crop up in extranodal sites. As described earlier, the nuclei are very irregular in contour, with cleared-out or vesicular chromatin leaving a prominent nucleolus and thick nuclear rim (Figure 21.4). Folded, or cleaved, nuclei are common. The cells may have more cytoplasm than lymphocytes, and therefore a lower nuclear/cytoplasmic ratio.
弥漫大B细胞淋巴瘤通常不会误认为良性;因为核太异常。然而,它可能误认为其他类型恶性肿瘤,特别是考虑到它有发生在结外的倾向。如前所述,细胞核轮廓非常不规则,染色质透明或空泡状,留下突出的核仁和较厚的核膜边缘(图21.4)。常见折叠的或有裂的核。胞质可能比淋巴细胞多,因此核/质比较低。
Anaplastic large cell lymphoma is the T-cell equivalent of DLBCL. It is known for having even more elaborately folded nuclei, described as cerebriform, but still must be differentiated by T-specific markers.
间变性大细胞淋巴瘤是与DLBCL对应的T细胞肿瘤。众所周知,它有更精细的折叠核,称为脑回状核,但仍必须通过T细胞特异性标记加以区分。
Although at the time of this writing, DLBCL is largely a single category in the World Health Organization classification, the splitters are gaining on it. One emerging division is between those DLBCLs that are of germinal center cell origin, such as follicular lymphoma gone bad, and those of activated B-cell origin. The latter have the worse prognosis.
尽管在编写本书时,DLBCL在WHO分类中主要是单个类别,但正在尝试进一步分类。一个新出现进一步方法是生发中心细胞来源(如,滤泡性淋巴瘤)的DLBCL和活化B细胞来源的DLBCL。后者预后较差。
滤泡性淋巴瘤(Follicular Lymphoma)
Follicular lymphoma is the second-most common non-Hodgkin’s lymphoma. Together DLBCL and follicular lymphoma account for over half of the non-Hodgkin’s lymphomas. Follicular lymphoma is defined by a translocation in which bcl-2 (an anti-apoptotic factor) is abnormally upregulated. bcl-2 usually turns off in germinal centers, making the centroblasts and centrocytes susceptible to apoptosis. Abnormal retention of bcl-2 leads to cells that do not die, more or less, hence the malignancy. Follicular lymphoma appears as a nodular proliferation of back-to-back neoplastic follicles that fill the lymph node (Figures 21.5 and 21.6). Within these follicles are a mixture of neoplastic centrocytes (smaller) and centroblasts (larger); the relative proportion determines the grade of the lymphoma. Follicular lymphoma can also have areas of diffuse growth (the opposite of nodular), can spread to the marrow, and can transform to DLBCL. When circulating as a leukemia, the folded (cleaved) centrocyte nucleus has been compared to a “baby’s butt.”
滤泡性淋巴瘤是第二常见的非霍奇金淋巴瘤。DLBCL和滤泡性淋巴瘤加起来超过非霍奇金淋巴瘤的一半。滤泡性淋巴瘤的遗传学特征是一种异位,导致bcl-2(一种抗凋亡因子)异常上调。bcl-2通常在生发中心关闭,使中心母细胞和中心细胞容易凋亡。易位导致bcl-2不关闭,细胞在一定程度上不死亡,因此导致恶性肿瘤。滤泡性淋巴瘤表现为背靠背的肿瘤性滤泡呈结节状增生,充满淋巴结(图21.5和21.6)。在这些滤泡内,肿瘤性中心细胞(较小)和中心母细胞(较大)混合存在;二者相对比例决定了淋巴瘤的分级。滤泡性淋巴瘤也可以有弥漫性生长区(与结节相反),可以扩散到骨髓,并可以转化为DLBCL。出现在循环中表现为白血病时,折叠(有核裂)的中心细胞核就像“婴儿屁股”。
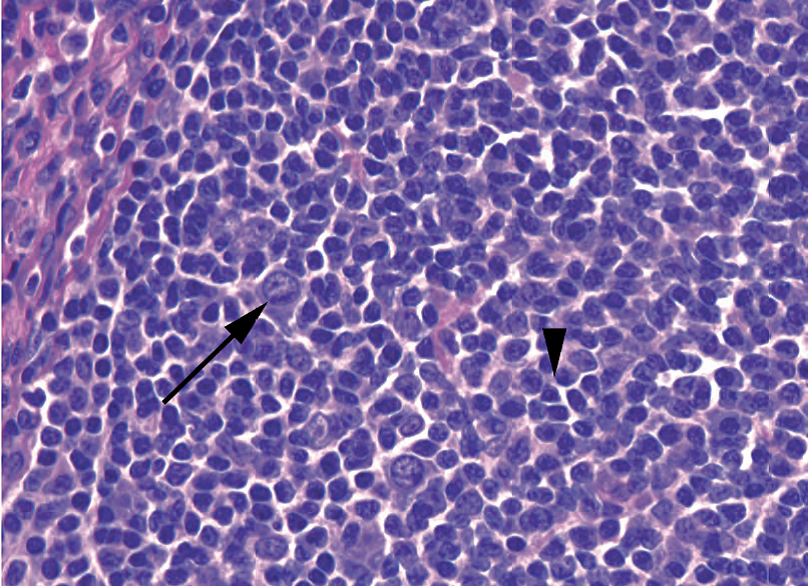
Figure 21.5. Follicular lymphoma. The lymph node is replaced by malignant follicles (arrows), which lack the mantle zones, polarization, and cell heterogeneity of germinal centers.
图21.5 滤泡性淋巴瘤。淋巴结被恶性滤泡(箭)取代,这些滤泡缺乏正常生发中心的套区、极性和细胞异质性。
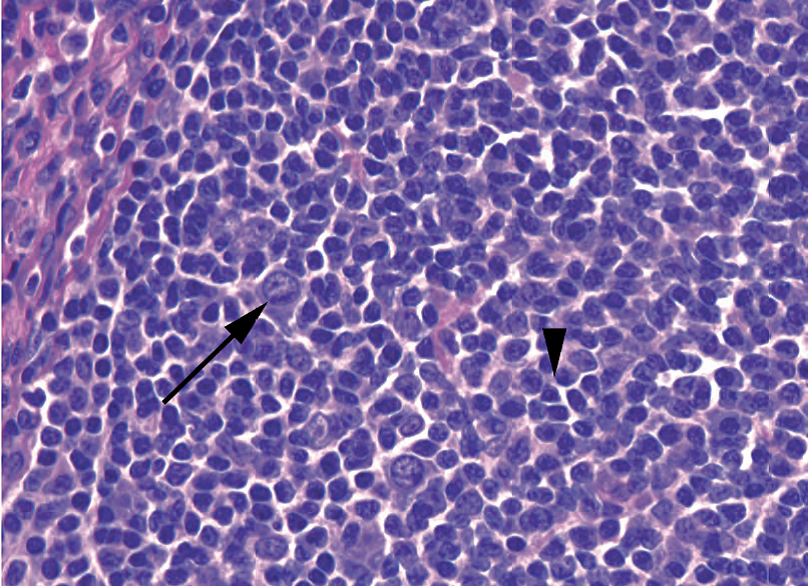
Figure 21.6. Follicular lymphoma, high power. The malignant follicles contain a mixture of small cleaved centrocytes (arrowhead) and large centroblasts (arrow).
图21.6 滤泡性淋巴瘤,高倍。恶性滤泡含有小裂中心细胞(箭头)和大的中心母细胞(箭)的混合物。
The diagnostic dilemma is that benign, reactive lymphoid hyperplasia can also present as a nodular collection of follicles in an enlarged node. How to distinguish the two? The following are features of benign follicular hyperplasia, not seen in follicular lymphoma (see Figures 21.1 and 21.2):
诊断难题是良性反应性淋巴增生也可以表现为肿大淋巴结中的结节状滤泡增生。如何区分两者?以下是良性滤泡增生的特征,未见于滤泡性淋巴瘤中(见图21.1和21.2):
Germinal centers of variable sizes and cuffed by mantle zones (as opposed to back to back)
生发中心大小不一,有套区(而不是背靠背)
Polarity of germinal centers in which the centroblasts and centrocytes tend to take up opposite positions in the follicle, creating an asymmetry
生发中心有极性,中心母细胞和中心细胞倾向于在滤泡中占据相反的位置,造成不对称
Tingible body macrophages
可染小体巨噬细胞
“Open” sinuses (which are not seen as open, really, but full of histiocytes)
“开放的”窦(实际上并不开放,而是充满组织细胞)
Abundant mitoses and apoptoses
丰富的核分裂和凋亡
These features should weed out the most straightforward cases. However, in very tough cases, stains help. The neoplastic follicles of follicular lymphoma can be stained with bcl-2; benign follicles should be negative.
这些特性应该可以排除最简单的病例。然而,在非常困难的病例中,免疫染色会有帮助。滤泡性淋巴瘤的肿瘤滤泡呈bcl-2阳性;良性滤泡应为阴性。
其他低级别B细胞肿瘤(Other Low-Grade B-Cell Neoplasms)
The other three most common low-grade lymphomas, small lymphocytic lymphoma (SLL), mantle cell lymphoma (MCL), and marginal zone lymphoma (MZL), each make up less than 10% of non-Hodgkin’s lymphomas. For these, and actually for most non-Hodgkin’s lymphomas, flow cytometry is critical in the diagnosis. Flow cytometry can establish two things:
其他三种最常见的低级别淋巴瘤,小淋巴细胞淋巴瘤(SLL)、套细胞淋巴瘤(MCL)和边缘区淋巴瘤(MZL),各占非霍奇金淋巴瘤的10%以下。对于这些肿瘤,实际上对于大多数非霍奇金淋巴瘤,流式细胞术在诊断中是至关重要的。流式细胞术可以确定两件事:
That there is a monoclonal population present. All B cells express either kappa or lambda light chain, so a significant predominance of one or the other implies a large genetically identical population (a neoplasm). A similar test can be done for T-cell neoplasms (T-cell receptor rearrangement studies) but not by flow cytometry.
存在单克隆细胞群。所有B细胞都表达kappa或lambda轻链,因此,其中一个占据显著优势意味着遗传学上相同的大量细胞群(肿瘤)。T细胞肿瘤也可以进行类似的检测(T细胞受体基因重排)。
That there are cells with an abnormal phenotype. The power of flow cytometry is that individual cells can be simultaneously tested for multiple markers, for instance, abnormal coexpression of CD20 and CD5. Doing this with immunohistochemistry is much less precise; you can estimate that the CD5+ cells outnumber the normal T cells (identified by CD3) and that they are clustered in areas of B cells (identified by CD20), but you cannot see two markers on a single cell.
存在异常表型的细胞。流式细胞术的优点在于可以同时检测单个细胞的多种标记物,例如,CD20和CD5的异常共表达。相比之下,免疫组织化学不太精确;你可以估计CD5+细胞的数量超过正常T细胞(由CD3识别),并且它们聚集在B细胞区域(由CD20识别),但你无法在单个细胞上看到两个标记。
The interpretation of flow cytometry is beyond the scope of this chapter, but the major learning point is that saving tissue for flow cytometry will make your life much easier, so set some aside in any lymphadenopathy workup or possible extranodal lymphoma. Formalinized (fixed) tissue cannot be sent for flow cytometric studies.
流式细胞术的解读超出了本章的范围,但主要的学习点是,保留新鲜组织用于流式细胞术将使你的生活更加轻松,因此在任何淋巴结病检查或可能的结外淋巴瘤中留出一些样本。不能将福尔马林固定组织送检流式细胞术。
In the low-grade B cell lymphomas, the low-power feature that rings alarm bells is the effacement of the lymph node. This means that the normal architecture, the follicles and sinuses and interfollicular areas, have been blurred out or replaced by a rather uniform population of cells. This takes some experience to judge; fortunately, every carcinoma resection comes with some bonus lymph nodes, so take the time to notice what normal looks like.
在低级别B细胞淋巴瘤中,拉响警铃的低倍特征是淋巴结结构消失。这意味着正常的结构,即滤泡、窦和滤泡间区域,已经模糊或被相当均匀的细胞群所取代。这需要一些经验来判断;幸运的是,每一次癌切除术都会有一些额外的淋巴结,所以花点时间学习正常形态学。
小淋巴细胞淋巴瘤(Small Lymphocytic Lymphoma)
Small lymphocytic lymphoma is the solid-phase manifestation of chronic lymphocytic leukemia, and the two are often seen in concert. In lymphoma form, SLL appears at 1× as a
very homogeneous, very blue lymph node. At low power, the follicles, paracortex, and sinuses are replaced by a sheet of what look like normal lymphocytes. There may be a vague suggestion of nodularity, called pseudofollicles, containing proliferating cells (Figure 21.7). On high power, the SLL cells usually have chromatin that may remind you of a plasma cell; they look like soccer balls. The nuclei are small, round, regular, and without nucleoli. Small lymphocytic lymphoma cells express CD23 and CD5.
小淋巴细胞淋巴瘤是慢性淋巴细胞白血病的实体肿瘤表现,二者常同时出现。在淋巴瘤形式中,SLL在1×镜下显示非常均匀、非常蓝染的淋巴结。低倍镜下,滤泡、副皮质和窦被一大片看似正常的淋巴细胞所取代。可能有一种模糊的结节性感觉,称为假滤泡,含有增殖细胞(图21.7)。在高倍镜下,SLL细胞的染色质通常可能会让你想起浆细胞;它们看起来像足球。细胞核小,圆,规则,无核仁。小淋巴细胞淋巴瘤细胞表达CD23和CD5。
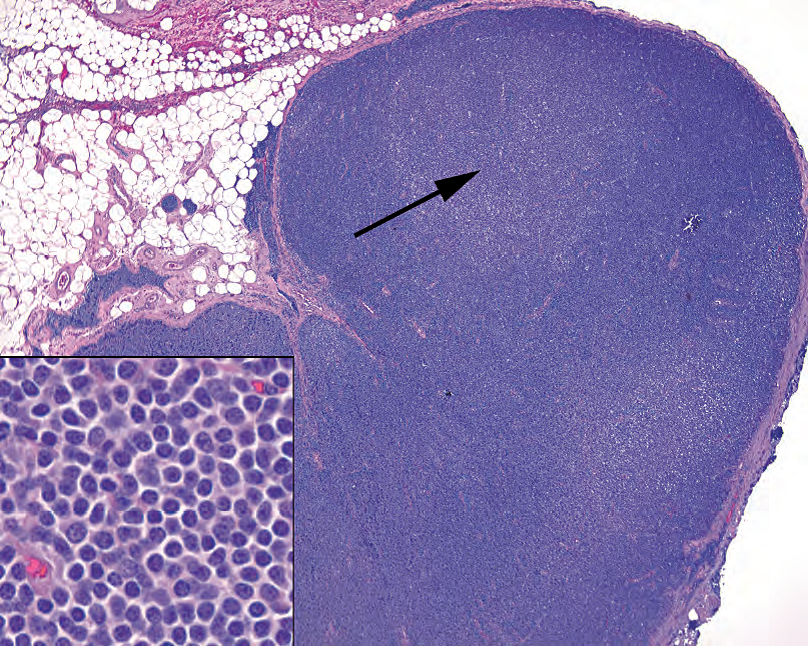
Figure 21.7. Small lymphocytic lymphoma. The lymph node, at low power, is an unnatural flat blue, without the variegation of normal sinuses and follicles. Subtle pale pseudofollicles (arrow) may be seen. Inset: The cells are small and nuclei are round and dense, like normal lymphocytes, except the chromatin has a chunky soccer-ball pattern, similar to a plasma cell.
图21.7 小淋巴细胞淋巴瘤。低倍镜下,淋巴结呈现不自然的淡蓝色,没有正常的窦和滤泡所形成的杂色。可以看到细微的淡染假滤泡(箭)。插图:细胞小,细胞核圆而致密,像正常淋巴细胞,只是染色质呈粗糙的足球状,类似于浆细胞。
套细胞淋巴瘤(Mantle Cell Lymphoma)
Mantle cell lymphoma, although it is in the histologic differential diagnosis for the low-grade lymphomas, actually behaves more aggressively than the others in this group. On low power it is reminiscent of SLL, with sheets of small lymphocytes effacing the node. In a not-entirelyreplaced node you may be able to tell that the mantle zones are expanding to engulf the germinal centers. Hyalinized vessels are typical. On high power, the cells of MCL have a chunky dark chromatin similar to the cells of SLL, but the nuclear membranes are more crinkled or angular, with more size variation (Figure 21.8). Cyclin D1 is the marker for MCL, which correlates with the translocation that defines the tumor.
套细胞淋巴瘤,虽然属于低级别淋巴瘤的组织学鉴别诊断范围,但实际上其侵袭性比该组的其他淋巴瘤更强。在低倍镜下,它让人联想到SLL,成片的小淋巴细胞取代淋巴结。在一个尚未完全取代的淋巴结中,你可能看出套区正在扩张,吞没生发中心。透明变性的血管是典型的表现。在高倍镜下,MCL细胞与SLL细胞具有类似的深染的粗块状染色质,但核膜更起皱或成角,核大小变化更大(图21.8)。Cyclin D1是MCL的标记物,与肿瘤特征性遗传学易位相关。

Figure 21.8. Mantle cell lymphoma. The neoplastic cells in mantle cell tend to be more irregular in shape than those of small lymphocytic lymphoma, with slightly angular nuclei. The chromatin pattern, with the soccer-ball splotches, is similar to small lymphocytic lymphoma.
图21.8 套细胞淋巴瘤。与小淋巴细胞性淋巴瘤相比,肿瘤细胞形状往往更不规则,核稍微成角。带有足球样斑点的染色质模式类似于小淋巴细胞淋巴瘤。
边缘区淋巴瘤(Marginal Zone Lymphoma,MZL)
The marginal zone of the lymph nodes is named for the more prominent and identifiable marginal zone in the spleen. In the lymph nodes, it is barely visible as a slightly attenuated zone surrounding the mantle. The cells in this zone have a prominent rim of clear cytoplasm, giving them almost a fried-egg appearance, and a pale look at low power. This morphology is called monocytoid. This cell type can give rise to at least three distinct lymphomas: splenic MZL (not discussed here), nodal MZL, and extranodal mucosa-associated lymphoid tissue (MALT) lymphoma of gut, salivary glands, and so forth.
淋巴结的边缘区因脾脏中更明显、更容易识别的边缘区而命名。在淋巴结中,它几乎无法辨认,只是套区周围的一个轻微淡染的区域。边缘区细胞有一圈明显的透明细胞质边缘,几乎像煎鸡蛋的样子,低倍镜下淡染。这种形态称为单核细胞样。这种细胞类型至少可导致三种不同的淋巴瘤:脾脏MZL(此处未讨论)、淋巴结MZL,以及肠道、唾液腺等淋巴结外粘膜相关淋巴组织(MALT)的淋巴瘤。
MALT lymphomas are discussed in Chapter 7. Like MALT lymphomas, the cells of MZLs are monocytoid in appearance and grow in sheets or clusters, mainly in the interfollicular
areas (Figure 21.9). They are negative for most of the markers that identify other lymphomas but may sometimes abnormally express CD43.
MALT淋巴瘤在第7章中讨论。与MALT淋巴瘤一样,MZL细胞呈单核细胞样,成片或成簇生长,主要位于滤泡间区(图21.9)。识别其他淋巴瘤的标记物大多数呈阴性,但有时可能异常表达CD43。
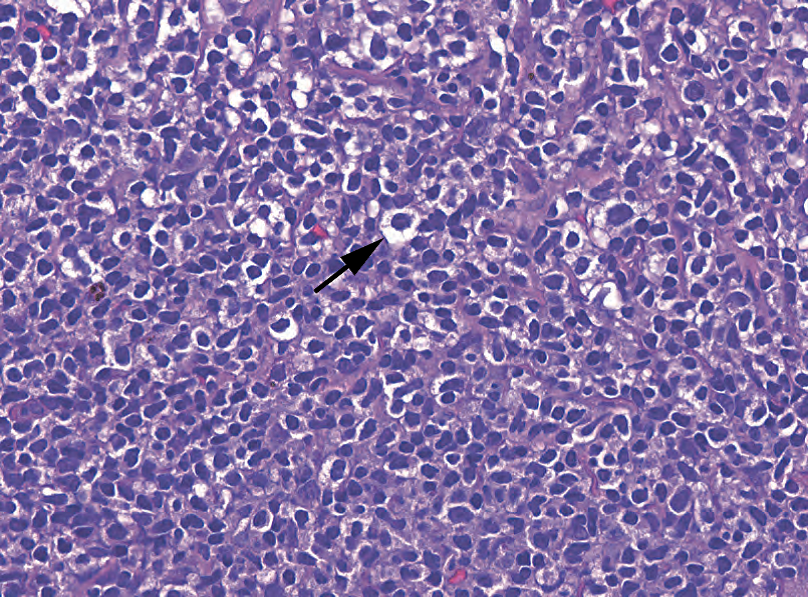
Figure 21.9. Marginal zone lymphoma. The marginal zone cells classically have a monocytoid appearance, meaning there is a distinct thin halo of clear cytoplasm (arrow).
图21.9 边缘区淋巴瘤。边缘区细胞通常呈单核细胞样外观,这意味着有明显的薄薄的一圈透明细胞质(箭)。
标记物(Markers)
Although the low-grade B-cell lymphomas do have histologic features that distinguish them, few pathologists would sign them out without confirming flow cytometry or immunostain studies. Although this book does not otherwise focus on immunostains, it is impossible to discuss the lymphomas without them. The standard panel includes CDs 3 and 20, 5 and 10, and 43, as well as some specific markers discussed earlier. CD3 identifies T cells, and CD20 identifies B cells. The expression of either CD5 or CD43, (T-cell markers), or CD10, (an immature B-cell/germinal center marker), in mature B cells is abnormal, and guides your differential.
尽管低级别B细胞淋巴瘤确实具有可以区分它们的组织学特征,但很少有病理学家会在不用流式细胞术或免疫染色进一步确认的情况下签发报告。虽然本书不关注免疫染色,但没有它就不可能讨论淋巴瘤。标准组合包括CD3、CD20、CD5和CD10和CD43,以及前面讨论的一些特定标记物。CD3识别T细胞,CD20识别B细胞。成熟B细胞表达CD5或CD43(T细胞标记物)或CD10(未成熟B细胞/生发中心标记物)属于异常表达,会指导你的鉴别诊断。
淋巴母细胞淋巴瘤(Lymphoblastic Lymphoma,LBL)
The lymphoblastic lymphomas are not usually diagnosed in lymph nodes. The precursor-B type more commonly presents as a leukemia (acute lymphoblastic leukemia), whereas the precursor-T type is most often seen as a mediastinal mass (remember the immature T cells are found in the thymus; Figure 21.10). Burkitt’s lymphoma is also in this category, and the cells are similar in appearance; it may present anywhere, especially in the gut. Most acute lymphoblastic leukemias are now defined by cytogenetics, but they also stain for the blast markers TdT and CD34 (Burkitt’s lymphoma not included). As CD45, the usual screening immunostain, is not reliably expressed in these tumors, be aware that a negative CD45 in a pediatric small round blue cell tumor may still be lymphoma. Finally, what looks like a lowgrade B-cell lymphoma in a child is much more likely to be a lymphoblastic lymphoma.
淋巴母细胞淋巴瘤通常不在淋巴结中诊断。前B型LBL更常见于白血病(急性淋巴母细胞白血病),而前体T型LBL最常见于纵隔肿块(请记住,未成熟T细胞见于胸腺;图21.10)。伯基特淋巴瘤也属于这一类(常发生在结外或表现为白血病形式),并且细胞外观相似;它可能出现在任何地方,尤其是肠道。大多数急性淋巴母细胞白血病现在是由细胞遗传学定义的,但也表达原始细胞标记物TdT和CD34(不包括伯基特淋巴瘤)。由于CD45(通常的筛选免疫染色)在这些肿瘤中的表达不可靠,请注意,儿童小圆蓝细胞肿瘤呈CD45阴性可能仍然是淋巴瘤。最后,儿童的看似低级别B细胞淋巴瘤更可能是淋巴母细胞淋巴瘤。

Figure 21.10. Acute lymphoblastic lymphoma. The nuclei (arrow) are larger than a normal lymphocyte (arrowhead), and the chromatin is very immature (meaning widely dispersed throughout the nucleus). Unlike large B-cell lymphoma, there are no prominent nucleoli or thick nuclear membranes.
图21.10 急性淋巴母细胞淋巴瘤。肿瘤细胞核(箭头)比正常淋巴细胞核(箭头)更大,染色质非常不成熟(意味着遍布在核中)。与大B细胞淋巴瘤不同,它没有明显的核仁或厚核膜。
霍奇金淋巴瘤(Hodgkin’s Lymphoma)
Hodgkin’s lymphoma is common, comprising 30%–40% of all lymphomas. It is now divided into two large groups, classic (most types) versus nodular lymphocyte predominant (NLPHL). Both groups share the histologic features of a dense and effacing mixed inflammatory infiltrate with scattered Reed-Sternberg (or Reed-Sternberg–like) cells. Because of the high benign background population, flow cytometry is not effective in detecting Hodgkin’s lymphoma. Making the diagnosis requires either seeing the diagnostic tumor cells or demonstrating them by immunostain. In classic Hodgkin’s lymphoma, the Reed-Sternberg cells are CD30 and CD15 positive while negative for CD45 and CD20. In NLPHL, the tumor cells stain exactly the opposite (45/20+, 30/15-). In this sense, NLPHL is really analogous to a DLBCL with an associated inflammatory response.
霍奇金淋巴瘤常见,占所有淋巴瘤的30%-40%。它现在分为两大类,经典型(大多数类型)和结节型淋巴细胞为主型(NLPHL)。二者具有共同的组织学特征:密集的、侵蚀的混合性炎性浸润,伴散在的RS(或RS样)细胞。由于含有大量的良性炎症背景,流式细胞术在检测霍奇金淋巴瘤方面并不有效。做出诊断需要看到诊断性肿瘤细胞或通过免疫染色显示它们。在经典型的霍奇金淋巴瘤中,RS细胞呈CD30和CD15阳性,而CD45和CD20阴性。在NLPHL中,肿瘤细胞的染色正好相反(CD45/20+,CD30/15-)。从这个意义上讲,NLPHL实际上类似于DLBCL伴炎症反应。
The subtypes of classic Hodgkin’s lymphoma include nodular sclerosing, mixed cellularity, and the less common lymphocyte depleted and lymphocyte rich. All should have some variety of the Reed-Sternberg cells, which in classic form have at least two nuclear lobes, each with a prominent, cherry-red nucleolus and thick nuclear membrane (Figure 21.11). However, variants with single or multilobed nuclei may be seen.
经典型霍奇金淋巴瘤有4种亚型:结节硬化型、混合细胞型、淋巴细胞消减型(少见)和淋巴细胞丰富型(少见)。所有亚型的都应该有一定数量的RS细胞,典型的RS细胞至少有两个核叶,每个核叶都有一个突出的樱桃红色核仁和厚核膜(图21.11)。然而,可以看到具有单叶或多叶核的变体。
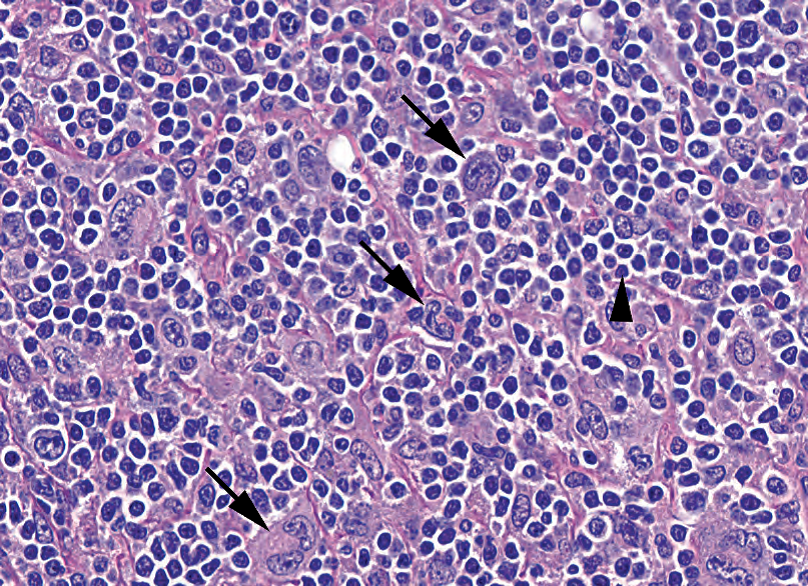
Figure 21.11. Hodgkin’s lymphoma. The malignant Reed-Sternberg cells (arrows) are spread out among a background of nonneoplastic inflammatory cells, especially lymphocytes (arrowhead).
图21.11 霍奇金淋巴瘤。恶性RS细胞(箭)散在分布于非肿瘤性炎症细胞背景中,炎症背景以淋巴细胞为主(箭头)。
In nodular sclerosing Hodgkin’s lymphoma, at low power, the node is “cirrhotic,” with nodules of mixed inflammation divided by broad fibrous bands (Figure 21.12). The node is usually also encapsulated. The Reed-Sternberg cells take the form of lacunar cells, which means the diagnostic nuclei are suspended in a retracted space or halo.
在结节硬化性霍奇金淋巴瘤中,低倍镜下,结节是“硬化的”,混合性炎症结节被宽广的纤维带分隔(图21.12)。结节通常也被纤维包裹。RS细胞呈陷窝细胞的形式,这意味着诊断性细胞核悬浮在收缩的空隙或空晕中。
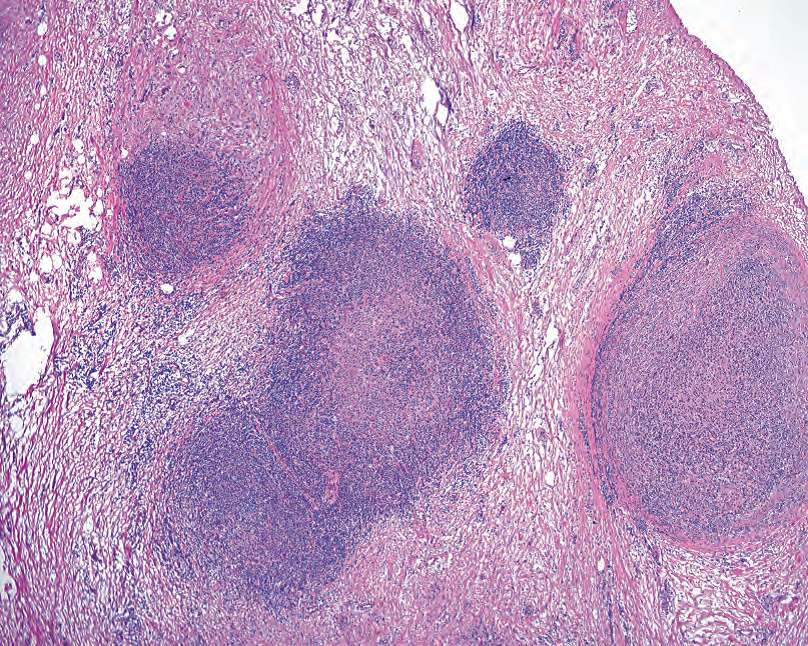
Figure 21.12. Nodular sclerosing Hodgkin’s lymphoma. The aggregates of Reed-Sternberg cells and inflammation are separated by broad bands of fibrosis.
图21.12 结节硬化性霍奇金淋巴瘤。RS细胞和炎症的聚集灶被宽广的纤维带分开。
At low power, mixed cellularity Hodgkin’s lymphoma appears “pink” because of the abundant histiocytes and eosinophils found in the background infiltrate (Figure 21.13). Plasma cells and lymphocytes are also common. Very subtle cases may present as granulomatous inflammation.
低倍镜下,混合细胞型霍奇金淋巴瘤呈“粉红色”,因为背景浸润中发现大量组织细胞和嗜酸性粒细胞(图21.13)。浆细胞和淋巴细胞也很常见。非常微妙的病例可能表现为肉芽肿性炎症。
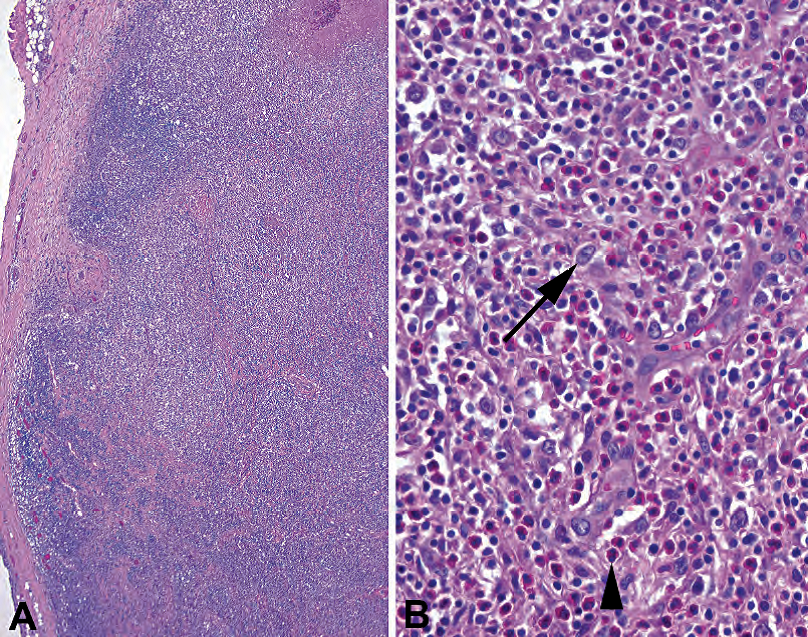
Figure 21.13. Mixed cellularity Hodgkin’s lymphoma. (A) At low power, the lymph node appears to be effaced by a heterogeneous population, giving a slightly pink color to the node (compare to small lymphocytic lymphoma in Figure 21.7). (B) The Reed-Sternberg variants are few and far between (arrow), with a dominant population of eosinophils (arrowhead).
图21.13 混合细胞性霍奇金淋巴瘤。(A)低倍镜下,淋巴结似乎被异质性细胞群所侵蚀,使淋巴结略呈粉红色(与图21.7中的小淋巴细胞淋巴瘤相比)。(B)RS变异体很少并且间隔很远(箭),嗜酸性粒细胞占优势(箭头)。
T细胞淋巴瘤(T-Cell Lymphomas)
The incidence of T-cell neoplasms is much lower than that of B cells. Precursor T-lymphoblastic lymphoma has been discussed, as has anaplastic large cell lymphoma. The cutaneous T-cell neoplasms include mycosis fungoides/Sezary syndrome (the solid and circulating phases, respectively) and primary cutaneous anaplastic large cell lymphoma. Of those that may present in a lymph node, peripheral T-cell lymphoma, unspecified, is the most common.
T细胞肿瘤的发病率远低于B细胞肿瘤。上文已经讨论了前体T淋巴母细胞淋巴瘤和间变性大细胞淋巴瘤。皮肤T细胞肿瘤包括蕈样肉芽肿/Sezary综合征(分别为实体瘤和循环期)和原发性皮肤间变性大细胞淋巴瘤。在可能出现在淋巴结中那些T细胞淋巴瘤中,非特指型外周T细胞淋巴瘤是最常见的。
非肿瘤实体(Nonneoplastic Entities)
Inflammation in a lymph node? It is only abnormal if it is granulomatous, acute, or necrotizing. Granulomatous inflammation may be nonnecrotizing in sarcoid or caseating in tuberculosis or fungal infection. Both of the latter should have positive findings on bug stains. Other infectious entities include infectious mononucleosis and cytomegalovirus, which can both cause dramatic follicular hyperplasia; cat scratch disease, causing an acute lymphadenitis with neutrophils; and Toxoplasma, which causes a follicular hyperplasia with ill-defined granulomatous inflammation. An unusual disease, called Kikuchi’s lymphadenitis, resembles a granulomatous response, with large swaths of geographic necrosis, but on high power the necrotic areas are paradoxically devoid of neutrophils, showing only apoptotic nuclear debris.
淋巴结炎?只有在肉芽肿性、急性或坏死性淋巴结炎,炎症才是仅有的异常。肉芽肿性炎可能表现为结节病中的非坏死性,也可能表现为结核病或真菌感染的干酪样。后二者都应该呈细菌染色阳性。其他感染性疾病包括传染性单核细胞增多症和巨细胞病毒,二者都能引起剧烈的滤泡增生;猫抓病,引起有中性粒细胞的急性淋巴结炎;弓形虫,引起滤泡增生和边界不清的(译注:虫蚀样)肉芽肿性炎症。一种被称为Kikuchi淋巴结炎的少见疾病,类似肉芽肿反应,伴有大片地图样坏死,但在高倍镜下,坏死区域却反常地没有中性粒细胞,仅显示凋亡的核碎片。
总结(Summary)

Knowledge of the pathway of B cells through the germinal centers, and the various markers that switch on and off, is very helpful in understanding the various B-cell neoplasms that arise from the different stages of maturation. The introductory chapter on mature B-cell neoplasms in the World Health Organization’s textbook Tumours of Haematopoietic and Lymphoid Tissues is a very good place to start.
了解B细胞通过生发中心的途径,以及B细胞发育过程中开启和关闭的各种标记物,对于理解不同成熟阶段产生的各种B细胞肿瘤非常有帮助。WHO分类书中关于成熟B细胞肿瘤的介绍性章节是非常好的学习起点。
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。
本站欢迎原创文章投稿,来稿一经采用稿酬从优,投稿邮箱tougao@ipathology.com.cn
相关阅读
 数据加载中
数据加载中
我要评论

热点导读
-

淋巴瘤诊断中CD30检测那些事(五)
强子 华夏病理2022-06-02 -

【以例学病】肺结节状淋巴组织增生
华夏病理 华夏病理2022-05-31 -

这不是演习-一例穿刺活检的艰难诊断路
强子 华夏病理2022-05-26 -

黏液性血性胸水一例技术处理及诊断经验分享
华夏病理 华夏病理2022-05-25 -

中老年女性,怎么突发喘气困难?低度恶性纤维/肌纤维母细胞性肉瘤一例
华夏病理 华夏病理2022-05-07






共0条评论