外科病理学实践:诊断过程的初学者指南 | 第20章 骨髓
第20章 骨髓(Bone Marrow)
正常组织学(Normal Histology)
The marrow biopsy specimen is usually taken from the iliac bone. It consists of bony trabeculae surrounded by a mixture of fat and hematopoietic cells. The percent cellularity (non-fat) should be roughly [100 – the patient’s age]. The hematopoietic cells consist of megakaryocytes, erythroid precursors, and myeloid precursors. There may also be assorted plasma cells, lymphocytes, and histiocytes. The bone marrow is considered a reflection of what is in the peripheral blood, so the disorders of marrow affect blood counts. Lymphomas can involve the marrow, but generally the primary malignancies of the marrow are the leukemias.
骨髓活检标本通常取自髂骨。它由骨小梁组成,周围是脂肪和造血细胞的混合物。细胞量百分比(非脂肪)应大致为[100–患者年龄]。造血细胞由巨核细胞、红系前体细胞和髓系前体细胞组成。也可能有混杂的浆细胞、淋巴细胞和组织细胞。骨髓反映外周血成分,因此骨髓疾病会影响血细胞计数。淋巴瘤可以累及骨髓,但通常骨髓的原发恶性肿瘤是白血病。
Technically, all three of the basic “trilineage hematopoiesis” lines (megakaryocytes, erythroids, and granulocytic cells) are of the myeloid lineage, which differentiates them from the lymphoid lineage (B and T cells). The myeloproliferative diseases and myeloid leukemias refer to this broad classification. However, the word myeloid, as used at the microscope, generally refers to those cells in the granulocyte/monocyte pathway only.
从技术上讲,所有三个基本的“三系造血”系(巨核细胞、红系细胞和粒细胞)都属于髓系,以区别于淋系(B细胞和T细胞)。骨髓增殖性疾病和髓系白血病指的是这个广泛分类。然而,显微镜下使用的“髓样”一词通常仅指粒细胞/单核细胞途径中的细胞。
Megakaryocytes are most easily identified, with their lakes of pink cytoplasm and multilobated nuclei (Figure 20.1). Erythroid precursors have a distinct rim of clear cytoplasm and centrally located, perfectly round nuclei; as they mature, the nuclei become small and dense such that erythroid islands in the marrow look like handfuls of buckshot (see Figure 20.1). Myeloid cells make up almost everything else. Myeloid precursors have more open chromatin than the red cell precursors, more cytoplasm, and more convoluted nuclei as they mature. Mature neutrophils and eosinophils should be present in normal marrow. Blasts, the most primitive hematopoietic cells, can be difficult to identify on H&E stain. Lymphoid cells, especially immature, should generally not be found in the marrow, with the exception of hematogones (nonneoplastic B-cell precursors), which can be markedly increased in children.
巨核细胞最容易识别,它们有粉红色的胞质湖和多叶核(图20.1)。红系前体细胞有清晰的透明细胞质边缘和位于中心的完美圆核;随着成熟,核变小变致密,骨髓中的红系岛看起来像一把霰弹(见图20.1)。其他主要是髓样细胞。随着髓样前体的成熟,它比红细胞前体有更多的开放染色质、更多的细胞质和更卷曲的细胞核。正常骨髓中应有成熟的中性粒细胞和嗜酸性粒细胞。原始细胞是最原始的造血细胞,在HE染色切片上很难识别。淋巴细胞,尤其是未成熟细胞,通常不应在骨髓中发现,但血原细胞(非肿瘤性B细胞前体)除外,在儿童中可能显著增多。
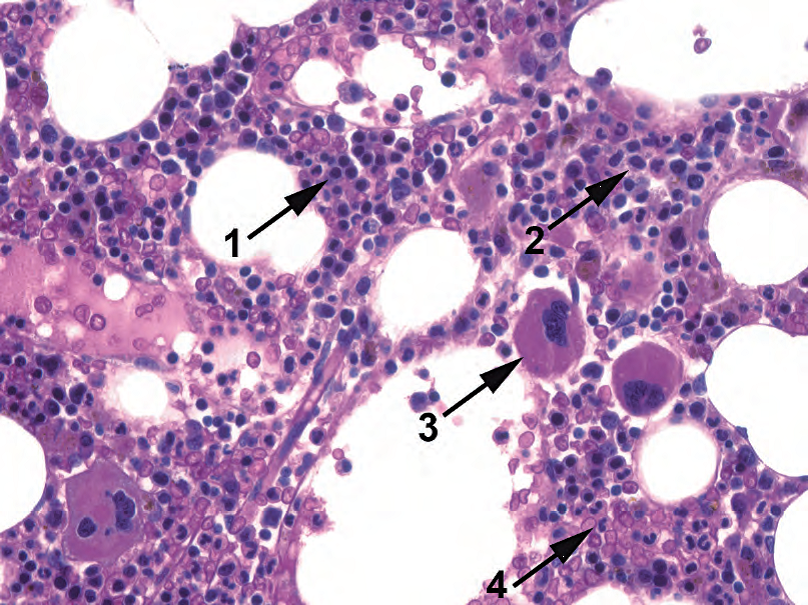
Figure 20.1. Normal megakaryocytes, erythroids, and myelocytic precursors. In this H&E stained core biopsy specimen, there are erythroid precursors (1), myeloid precursors (2), megakaryocytes (3), and maturing neutrophils (4).
图20.1 正常巨核细胞、红系和髓系前体。在HE染色的粗针活检标本中,有红系前体(1)、髓系前体(2)、巨核细胞(3)和成熟过程的中性粒细胞(4)。
Usually an aspirate smear will be submitted with the biopsy specimen. The aspirate is stained with the Wright-Giemsa stain, which highlights nuclear detail. Blasts, and the successive stages of maturation, are best seen on an aspirate. The blasts are large cells with a thin rim of cytoplasm and a characteristic nucleus (Figure 20.2). The blast nucleus is large and round with a very finely textured chromatin pattern and a nonstaining nucleolus that shows up as a “hole” in the chromatin. The more differentiated precursors, such as promyelocytes and myelocytes, may have a similarly immature nucleus but acquire cytoplasmic features such as granules and a “hof” (the cleared-out Golgi zone in the cytoplasm, as in a plasma cell; see Figure 20.2).
通常,穿刺涂片与活检标本一起送检。穿刺涂片用Wright-Giemsa染色,突出显示核细节。原始细胞及其连续的成熟阶段在穿刺涂片上最容易观察。原始细胞为大细胞,边缘有薄薄的一圈胞质,有特征性细胞核(图20.2)。核大而圆,染色质模式非常纤细,核仁不着色,像是染色质上的“孔”。更分化的前体细胞,如早幼粒细胞和中幼粒细胞,可能有类似的未成熟核,但具备了细胞质特征,如颗粒和“晕”(细胞质中透明的高尔基区,如浆细胞;见图20.2)。

Figure 20.2. Blast on aspirate, Wright-Giemsa stain. The key to identifying a blast is the high nuclear to cytoplasm ratio and immature chromatin pattern, which consists of very finely grained, uniform chromatin with several nucleoli that show up as negative images on this stain (arrowhead). The immature cell nearby is a promyelocyte, which has the same nuclear qualities as a blast but has abundant cytoplasm with granules (arrow).
图20.2 骨髓涂片中的原始细胞,Wright-Giemsa染色。识别原始细胞的关键是高核质比和不成熟的染色质模式,由非常纤细的颗粒性、均匀的染色质和几个核仁组成,核仁在这种染色上不显色(箭头)。附近的未成熟细胞是一个早幼粒细胞,核质地与原始细胞相同,但细胞质丰富,有颗粒(箭)。
On the aspirate, a myeloblast (as seen in acute myeloid leukemia) cannot always be distinguished from a lymphoblast (as seen in acute lymphoblastic leukemia). However, the presence of granules or Auer rods identifies a blast as myeloid. Erythroblasts have royal blue cytoplasm and very round nuclei. Monocyte precursors tend to have greyer cytoplasm and a folded or creased nucleus.
在穿刺涂片上,并非总是能够区分原粒细胞(如急性髓系白血病所见)与淋巴母细胞(如急性淋巴母细胞白血病所见)。然而,存在颗粒或Auer小体可确定为髓样细胞。早幼红细胞有皇家蓝色的细胞质和非常圆的核。单核细胞前体往往有灰色的细胞质和折叠核或皱折核。
活检标本的处理方法(Approach to the Biopsy Specimen)
A full evaluation of the specimen requires an H&E stained core biopsy, a Wright-Giemsa stained aspirate, and a peripheral smear. Beginning with the biopsy:
全面评估标本需要HE染色的粗针活检、Wright-Giemsa染色的骨髓涂片和外周涂片。首先,观察活检切片:
On low power (4×)
低倍镜(4×)
Assess the cellularity of the marrow (Figure 20.3). A hypo- or hypercellular marrow will guide your differential diagnosis.
评估骨髓的细胞量(图20.3)。低细胞量或高细胞量的骨髓将指导你的鉴别诊断。
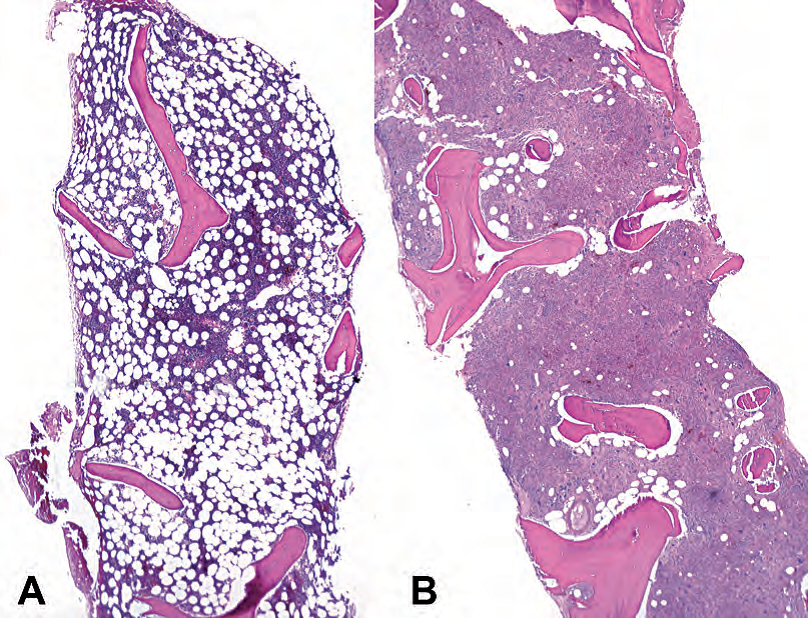
Figure 20.3. Marrow cellularity. (A) Normocellular marrow for a middle-aged adult; this cellularity is approximately 30%. (B) Hypercellular marrow for an adult; this cellularity is about 95% and is taken from a case of acute myeloid leukemia.
图20.3 骨髓细胞数。(A)中年成人,正常细胞量的骨髓;细胞量约为30%。(B)成人高细胞量的骨髓;细胞量约为95%,取自一例急性髓系白血病。
Try to estimate the cellularity as a percentage range (i.e., 30%–40%), as clinicians sometimes follow the cellularity to monitor response to therapy.
努力以百分比范围(即30%–40%)估计细胞量,因为临床医生有时会跟踪细胞量以监测治疗反应。
On medium power (10×)
中倍镜(10×)
Survey the marrow for trilineage hematopoiesis. You should see megakaryocytes, erythroid islands, and myeloid cells. Look to see if each line matures to completion: you should see mature neutrophils and red cells. Estimate the ratio of myeloid to erythroid cells (M/E ratio), which is normally about 2–4:1.
从总体上评估骨髓的三系造血。你应该看到巨核细胞、红系岛和髓系细胞。观察每个细胞系是否成熟到完全成熟:你应该看到成熟的中性粒细胞和红细胞。估计髓系细胞与红细胞的比率(M/E比率),通常约为2–4:1。
Look for things that do not belong in the marrow in large populations or aggregates, such as blue areas (lymphocytes), pink areas (histiocytes, plasma cells), or islands of non-heme cells (metastases). Look for fibrosis, which gives the marrow a streaming texture (Figure 20.4).
寻找骨髓不该大群或聚集的的东西,如蓝色区域(淋巴细胞)、粉红色区域(组织细胞、浆细胞)或非血细胞岛(转移)。寻找纤维化,它使骨髓呈流水样感觉(图20.4)。
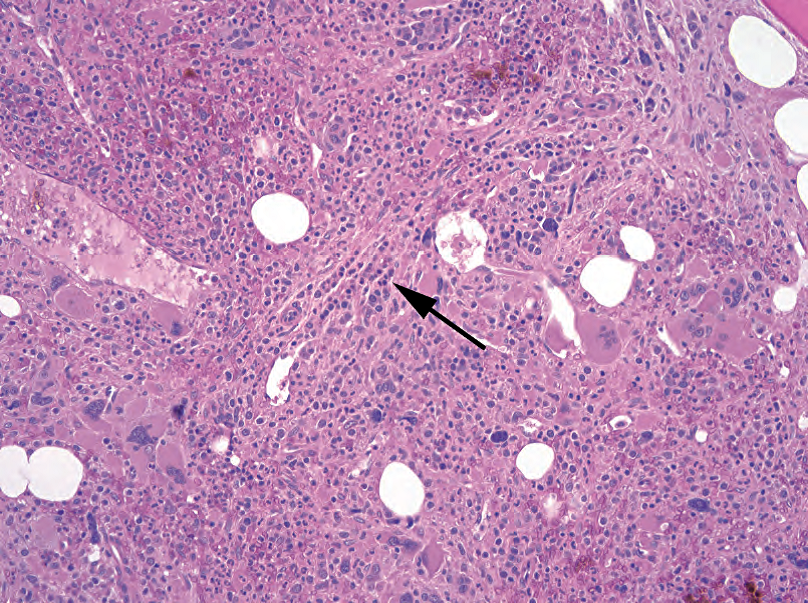
Figure 20.4. Marrow fibrosis. On hematoxylin and eosin stain, the marrow has a streaming texture (arrow), indicative of strands of collagen separating the hematopoietic cells into nests and channels.
图20.4 骨髓纤维化。HE染色,骨髓具有流动的感觉(箭),提示胶原束将造血细胞分隔成巢和通道。
On high power (20× and 40×)
高倍镜(20倍和40倍)
Look at the individual cells, especially megakaryocytes. Small megakaryocytes with single nuclei are a feature of myelodysplasia and are also seen in chronic myeloid leukemia (Figure 20.5). Giant clustered megakaryocytes are a feature of myeloproliferative disorders. A few atypical megakaryocytes are not unusual, but a large population is significant.
观察单个细胞,尤其是巨核细胞。单核的小巨核细胞是骨髓增生异常的特征,也可见于慢性髓系白血病(图20.5)。巨大成簇的巨核细胞是骨髓增殖性疾病的一个特征。少数非典型巨核细胞并不罕见,但形成大群是有意义的。
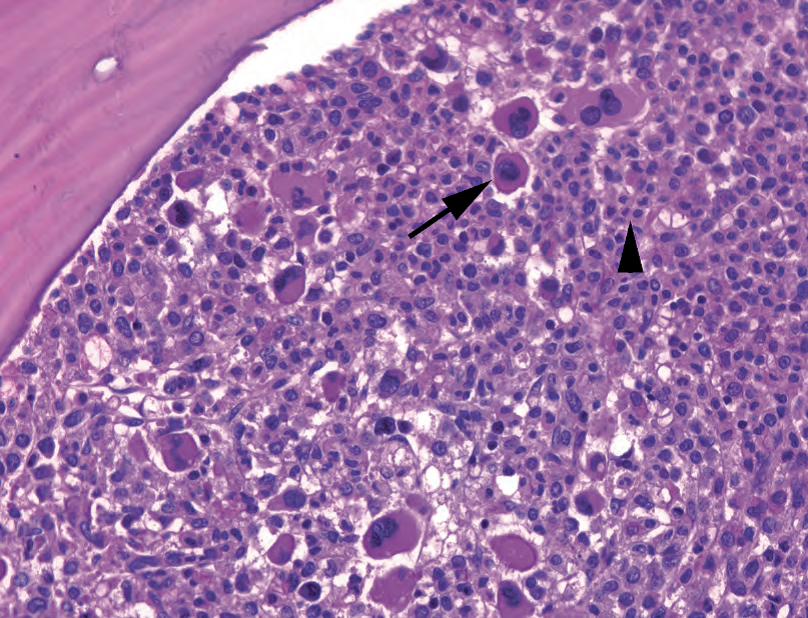
Figure 20.5. Chronic myeloid leukemia. This hypercellular marrow is full of small, hypolobated megakaryocytes (arrow) and maturing and mature neutrophils (arrowhead).
图20.5 慢性髓系白血病。这个高细胞量的骨髓标本充满了小的低分叶巨核细胞(箭),以及成熟过程中的和已成熟的中性粒细胞(箭头)。
Look for neutrophils. A packed marrow with numerous neutrophils may indicate chronic myeloid leukemia (see Figure 20.5), whereas numerous myeloid precursors with few neutrophils indicates a left-shift in maturation. Sheets of immature myeloid cells could represent anything from acute myeloid leukemia to infection; the aspirate needs to be evaluated for blasts (see next section).
寻找中性粒细胞。含有大量中性粒细胞的拥挤的骨髓可能提示慢性髓系白血病(见图20.5),而含有少量中性粒细胞的大量髓系前体则提示成熟度左移。成片的未成熟髓样细胞可能代表从急性髓系白血病到感染的任何东西;需要评估骨髓涂片有无原始细胞(见下一节)。
Next, look at the aspirate. Hold it up to the light; an adequate aspirate will have little chunks in it (spicules) that are foci of stromal elements. Scan the slide for an optimal area of the smear. Cells should be spread out in a monolayer, with intact cytoplasm and distinct nuclei. “Naked” nuclei are not evaluable.
然后,观察骨髓涂片。把它举到灯光下;标本量充分的涂片中会有小块状物(针状物),它们是小灶间质成分。扫描幻灯片,寻找涂片的最佳区域。细胞应呈单层分布,细胞质完整,细胞核清晰。“裸”核是不可评价的。
You have already evaluated the megakaryocytes, so, with the aspirate, focus on erythroid and myeloid cells. On high power (20× to 100×, with oil if necessary):
你已经评估了巨核细胞,因此,涂片重点是红系和髓系细胞。在高倍镜下(20×到100×之间,必要时用油镜):
Assess the heterogeneity of the marrow. A healthy aspirate should be a random mosaic of all different cell types at all levels of maturity. Sheets of uniform cells is a bad, bad sign (Figure 20.6).
评估骨髓的异质性。一个健康的涂片应该是所有成熟度水平的所有不同细胞类型的随机镶嵌。成片的均匀的细胞是糟糕的迹象(图20.6)。
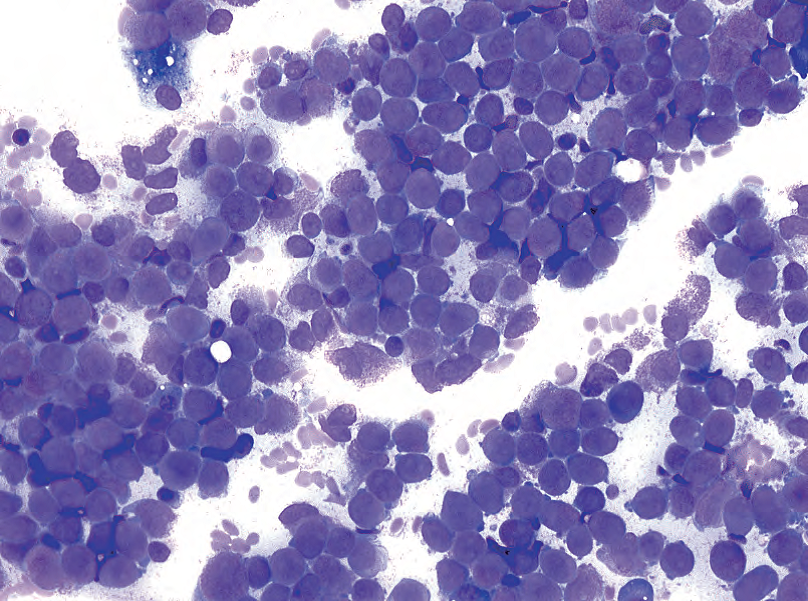
Figure 20.6. Monomorphic aspirate in acute leukemia. This aspirate is composed of sheets of blasts, identified by high nuclear to cytoplasmic ratios and immature chromatin.
图20.6 急性白血病的单形性涂片。这例涂片由成片的原始细胞组成,通过高核质比和未成熟的染色质来识别。
Look for blasts. You should be able to find scattered blasts but not clusters of them. Clumps of immature-looking cells are more commonly promyelocytes and myelocytes, as identified by their granules and cytoplasmic hofs. If you do find lots of blasts, note the shape of the nuclei, the color of the cytoplasm, and the presence of Auer rods. Presence of greater than 5% blasts is abnormal; they should be quantified by a systematic cell count of 200–500 cells. Flow cytometry will also provide a quantified percentage.
寻找原始细胞。你应该能够找到分散的原始细胞,但不能成簇分布。聚集的看似未成熟细胞通常是早幼粒细胞和中幼粒细胞,通过其颗粒和胞质空晕来识别。如果你确实发现了大量原始细胞,注意核形状,胞质颜色,有无Auer小体。原始细胞大于5%是不正常的;应全面计数200–500个细胞对其进行量化。流式细胞术也能提供定量百分比。
Evaluate the red cell precursors for dysplasia. Dyserythropoiesis shows up as binucleated red cells and red cell precursors with irregular nuclear membranes (Figure 20.7). Megaloblastoid change is a softer sign and looks like large “sliced salami” nuclei within mature (pale grey) cytoplasm.
评估增生异常的红细胞前体。红细胞生成障碍表现为双核红细胞和核膜不规则的红细胞前体(图20.7)。巨幼改变是一种较软的征象(译注:需要小心解读),看起来像成熟(浅灰色)细胞质内的大“切片萨拉米”细胞核。
(dysplasia血液病传统翻译“发育不良”。非血液病翻译“异型增生”。)
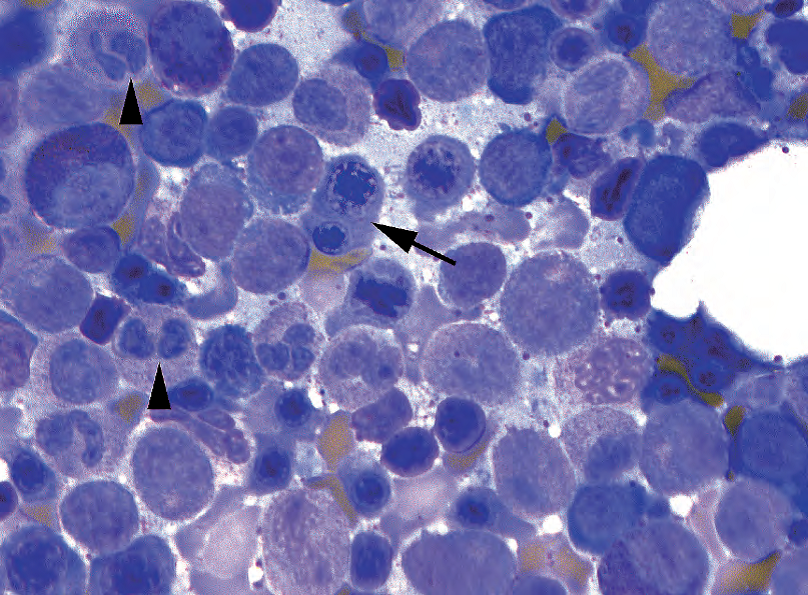
Figure 20.7. Dyserythropoiesis and dysgranulopoiesis. Binucleated erythroid precursors (arrow) and bilobed neutrophils without granules (arrowheads) are indicative of dysplasia.
图20.7 红细胞生成障碍和粒细胞生成障碍。双核红系前体细胞(箭)和无颗粒的双叶中性粒细胞(箭头)提示增生异常。
Dysgranulopoiesis (in neutrophils) appears as abnormalities in nuclear lobation (“Pelgeroid,” which is bilobed like spectacles) and granules (absence of granules or occasionally coarse basophilic granules). Hypersegmented neutrophils can be seen in megaloblastic anemia.
粒细胞生成障碍(在中性粒细胞中)表现为核分叶异常(“沙皮样”,类似双叶眼镜)和颗粒导演(缺乏颗粒或偶有粗糙的嗜碱性颗粒)。巨幼细胞性贫血中可见过度分叶的中性粒细胞。
Plasma cells are easy to spot on the aspirate, with their bright blue cytoplasm and eccen-tric nucleus. Too many plasma cells (more than 5%–10%) may indicate a plasma cell dyscrasia.
涂片中容易发现浆细胞,胞质呈鲜蓝色,核偏位。太多浆细胞(超过5%–10%)可能表明浆细胞异常。
Iron stains are performed on marrow smears to evaluate the iron stores. Hemosiderin (stainable storage iron) is found in reticuloendothelial cells and also in granules in normoblasts (developing red cell precursors). Normoblasts with iron granules in the cytoplasm are called sideroblasts. Sideroblasts are decreased in iron-deficiency anemia but increased in sideroblastic anemia, especially in the form of ringed sideroblasts, which have iron granules surrounding the nucleus in a ring.
骨髓涂片铁染色以评估铁储存。含铁血黄素(可染色储存铁)见于网状内皮细胞中,也见于晚幼红细胞(发育中的红细胞前体)的颗粒中。细胞质含有铁颗粒的晚幼红细胞称为铁粒幼细胞。缺铁性贫血中的铁粒幼细胞减少,而铁粒幼细胞性贫血中的铁粒幼细胞增多,尤其是环状铁粒幼细胞,铁颗粒围绕细胞核形成一个环。
After the aspirates, look at the peripheral blood film. Assess the white count, get a very rough differential, look for circulating blasts, and estimate the platelet count. (This chapter will not go into detail on peripheral smear interpretation.) Hypersegmented, hyposegmented, or hypogranular neutrophils are considered evidence of dysgranulopoiesis on the smear.
观察涂片后,再观察外周血片。评估白细胞计数,获得一个非常粗略的分类计数,寻找循环血中的原始细胞,并估计血小板计数。(本章将不详细介绍外周血片的解释。)过度分叶的、过少分叶的或低颗粒的中性粒细胞视为血片粒细胞生成障碍的证据。
鉴别诊断(Differential Diagnosis)
Once you have looked at everything, gather your facts to generate a differential diagnosis:
观察过所有内容后,收集你的发现,形成鉴别诊断:
Hypercellular or hypocellular? (See marrow cellularity)
高细胞量还是低细胞量?(见骨髓细胞量)
Dysplasia of any cell lines? (See myelodysplastic syndrome)
任何细胞系的增生异常?(见骨髓增生异常综合征)
A prominent excess of any one cell line? (See myeloproliferative disorders)
任何一个细胞系的显著过多?(见骨髓增殖性疾病)
Too many blasts? (See acute leukemia)
原始细胞太多了?(见急性白血病)
Lots of plasma cells? (See plasma cell dyscrasias)
很多浆细胞?(见浆细胞异常)
Lymphocytes? (See lymphoma)
淋巴细胞?(见淋巴瘤)
骨髓细胞量(Marrow Cellularity)
With hypercellular marrow, the differential diagnosis includes the following:
对于高细胞量的骨髓,鉴别诊断包括:
Physiologic response to anemia, especially hemolytic anemia, or infection (no dysplasia, no increase in blasts)
对贫血(尤其是溶血性贫血)或感染的生理反应(无增生异常,无原始细胞增多)
Ineffective hematopoiesis (such as megaloblastic anemia, human immunodeficiency virus)
无效造血(如巨幼细胞性贫血、人类免疫缺陷病毒)
Myelodysplasia (dysplastic hematopoiesis in any cell line, < 20% blasts)
骨髓增生异常(任何细胞系中的增生异常的造血,<20%的原始细胞)
Myeloproliferative disorders (chronic myeloid leukemia, polycythemia vera (PV), essential thrombocythemia (ET), myelofibrosis
骨髓增殖性疾病(慢性髓系白血病、真性红细胞增多症(PV)、原发性血小板增多症(ET)、骨髓纤维化
Acute leukemia (> 20% blasts, with or without dysplasia)
急性白血病(>20%的原始细胞,伴或不伴增生异常)
Other neoplasms (lymphoma, metastatic disease)
其他肿瘤(淋巴瘤、转移性疾病)
With hypocellular marrow, the differential diagnosis includes the following:
对于低细胞量的骨髓,鉴别诊断包括:
Aplastic anemia
再生障碍性贫血
Chemotherapy
化疗
Infection
感染
Hypocellular forms of myelodysplastic syndrome (MDS)/acute myeloid leukemia (blasts are still increased)
低细胞型骨髓增生异常综合征(MDS)/急性髓系白血病(原始细胞仍在增多)
(传统翻译:Marrow Cellularity骨髓增生程度。hypercellular marrow骨髓增生活跃。hypocellular marrow骨髓增生低下)
骨髓增生异常综合征(Myelodysplastic Syndrome)
Myelodysplastic syndrome includes the refractory anemia group of disorders and encompasses those diseases with dysplasia of at least one cell line AND with blasts < 20% in the marrow. Myelodysplastic syndrome often progresses to acute myeloid leukemia, which by definition is > 20% blasts. Each dysplastic cell line has a corresponding peripheral cytopenia, as it represents a dysfunctional hematopoiesis. Myelodysplastic syndrome tends to have an erythroid predominance in the marrow (decreased M/E ratio), as the body struggles to compensate for the anemia. The most minor disease is simple refractory anemia, which presents with anemia and shows erythroid dysplasia (see Figure 20.7). Blasts are not increased (< 5%). The finding of > 15% ringed sideroblasts on an iron stain indicates refractory anemia with ringed sideroblasts.
骨髓增生异常综合征(MDS)包括难治性贫血组疾病,并包括至少一个细胞系增生异常且骨髓中原始细胞<20%的疾病。骨髓增生异常综合征通常进展为急性髓系白血病,根据定义,急性髓系白血病的原始细胞>20%。每一个增生异常的细胞系都有相应的外周血细胞减少,因为它代表了功能失调的造血。骨髓增生异常综合征倾向于骨髓中以红系为主(M/E比率降低),因为身体努力对贫血做出代偿。最轻微的疾病是单纯性难治性贫血,表现为贫血和红系增生异常(见图20.7)。原始细胞未增多(<5%)。铁染色发现>15%的环形铁粒幼细胞提示难治性贫血伴环状铁粒幼细胞。
Dysplasia and cytopenias in two, or more usually three, cell lines bumps you to refractory cytopenia with multilineage dysplasia (with or without ringed sideroblasts). The dysplasia must be seen in > 10% of a given cell line to be significant. Blasts are still not increased.
增生异常和血细胞减少发生在两个或更多细胞系,通常是三系,促使你诊断难治性血细胞减少伴多系增生异常(伴或不伴环状铁粒细胞)。增生异常必须在特定细胞系中>10%才有意义。原始细胞仍然不增多。
Once the blast percentage begins to increase, you get to refractory anemia with excess blasts (RAEB)-1 or -2 for marrow blasts 5%–9% and 10%–19%, respectively. Refractory anemia with excess blasts is otherwise known as high-grade MDS and usually progresses to acute myeloid leukemia. The presence of an Auer rod in the setting of MDS, regardless of the percentage of blasts, indicates RAEB-2. Similarly, the presence of > 5% circulating or peripheral blasts indicates RAEB-2.
一旦原始细胞百分比开始增多,就是难治性贫血伴原始细胞增多(RAEB)-1或-2,其中骨髓原始细胞分别为5%-9%和10%-19%。RAEB又称为高级别MDS,通常进展为急性髓系白血病。无论原始细胞的百分比如何,MDS出现Auer小体提示RAEB-2。类似地,循环或外周原始细胞>5%提示RAEB-2。
骨髓增殖性疾病(Myeloproliferative Disorders)
The myeloproliferative disorders (MPDs), in contrast to myelodysplasia, show a superhematopoiesis. There is little or no dysplasia, and the peripheral counts of the involved cell line(s) are high. In chronic myeloid leukemia, the most common MPD, the polys are pushed out of the marrow so fast that they are not fully mature, so there are immature as well as mature granulocytes in circulation. Unlike MDS, there is an increased M/E ratio in the marrow. Like MDS, though, the marrow is hypercellular and the blast percentage is low (at least until it reaches a blast crisis). The gradual replacement of the bone marrow usually leads to cytopenias of the uninvolved cell lines (although chronic myeloid leukemia usually comes with a thrombocytosis), as well as extramedullary hematopoiesis and organomegaly.
骨髓增殖性疾病(MPD)与骨髓增生异常相反,表现为过度造血。很少或没有增生异常,受累细胞系的外周血计数高。在慢性髓系白血病(最常见的MPD)中,粒细胞被迅速推出骨髓,以至于它们尚未完全成熟,因此循环中存在未成熟和成熟的粒细胞。与MDS不同,骨髓M/E比率增加。不过,与MDS一样,骨髓为高细胞量,骨髓原始细胞百分比低(至少在骨髓原始细胞危象之前如此)。骨髓被逐渐替代,通常导致未受累细胞系的细胞减少(尽管慢性髓系白血病通常伴有血小板增多),以及髓外造血和器官肥大。
Myeloproliferative disorders can affect any of the myeloid (nonlymphoid) cell lines: granulocytic (chronic myeloid leukemia), megakaryocytic (essential thrombocythemia), and erythroid (polycythemia vera). Chronic idiopathic myelofibrosis involves both the megakaryocytic and granulocytic lines. The MPDs can have overlapping features and be difficult to separate, with the exception of chronic myeloid leukemia, which is defined by unique cytogenetics (t 9;22, bcr-abl, the Philadelphia chromosome).
骨髓增殖性疾病可影响任何髓系(非淋巴细胞)细胞系:粒系(慢性髓系白血病)、巨核系(原发性血小板增多症)和红系(真性红细胞增多症)。慢性特发性骨髓纤维化涉及巨核细胞系和粒细胞系。MPD可能具有重叠特征,难以分开,但慢性髓系白血病除外,它有独特的细胞遗传学(t 9;22,bcr abl,费城染色体)。
骨髓增生异常/骨髓增殖性疾病(Myelodysplastic/Myeloproliferative Disorders)
Of course there would be an overlap among the myelodysplastic and myeloproliferative disorders. The MDS/MPD category has features of both. The most common disorder is chronic myelomonocytic leukemia. It has the dysplasia, anemia, and thrombocytopenia of MDS, a proliferation of monocytes (monocytosis), < 20% blasts, and no Philadelphia chromosome.
当然,骨髓增生异常和骨髓增殖性疾病之间存在重叠。MDS/MPD类别兼有这两种特征。最常见的疾病是慢性粒单核细胞白血病。它有MDS的增生异常、贫血和血小板减少症,单核细胞增殖(单核细胞增多症),<20%的原始细胞,没有费城染色体。
急性白血病(Acute Leukemia)
Acute leukemia is defined as > 20% blasts in the blood or marrow, but it is not uncommon to see > 90% blasts in an initial presentation (Figure 20.8). Acute lymphoblastic leukemia (ALL) is the leukemic counterpart to acute lymphoblastic lymphoma and is primarily a disease of children in which immature lymphocyte precursors fill the marrow. Most commonly the cells are B-cell precursors (pre-B ALL), although T-cell ALL can also involve the marrow. Acute lymphoblastic leukemia can be very difficult to distinguish from acute myeloid leukemia on routine stains, as the lymphoblasts look very similar to myeloblasts. However, the diagnosis is easily confirmed by immunostains or flow cytometry.
急性白血病定义为血液或骨髓中原始细胞>20%,但初次就诊时原始细胞>90%并不少见(图20.8)。急性淋巴母细胞白血病(ALL)是急性淋巴母细胞淋巴瘤的白血病对应物,主要是一种儿童疾病,不成熟的淋巴细胞前体充满骨髓。最常见的是B细胞前体(前B ALL),尽管T-ALL也可累及骨髓。急性淋巴母细胞白血病在常规染色上很难与急性髓系白血病区分,因为淋巴母细胞很像原粒细胞。然而,免疫染色或流式细胞术很容易确诊。
Acute myeloid leukemia (AML) spans a wide category of diseases, which are roughly grouped by the type of blast that has gone bad. The classification of AML was by the FAB system for many years, which subgrouped the acute myeloid leukemias into the M0 to M7 categories (Table 20.1). The classification system used since 2001 is the World Health Organization (WHO) classification, which relies more on cytogenetic, molecular, and immunophenotypic features. In this system, some acute myeloid leukemias are defined by their cytogenetics, such as t(8;21) (ETO), t(15;17) (acute promyelocytic leukemia), and inv(16) (acute myelomonocytic leukemia with abnormal eosinophils). These are more likely to arise de novo and have a better prognosis. AML arising from MDS, however, has a poor prognosis and often deletions of chromosomes 5 and 7. Similar cytogenetics may be found in chemotherapy-related acute myeloid leukemia. The remaining AML subtypes include the leukemias previously defined in the FAB system, such as AML and acute megakaryoblastic leukemia.
急性髓系白血病(AML)囊括了广泛的疾病类别,这些疾病大致按照已经恶化的原始细胞类型进行分类。多年来,AML的分类一直采用FAB系统,该系统将急性髓系白血病再分为M0至M7类(表20.1)。自2001年以来使用的分类系统是世界卫生组织(WHO)的分类,它更多地依赖于细胞遗传学、分子和免疫表型特征。WHO分类中,一些急性髓系白血病是由其细胞遗传学定义的,如t(8;21)(ETO),t(15;17)(急性早幼粒细胞白血病)和inv(16)(急性粒单核细胞白血病伴异常嗜酸性粒细胞)。这些疾病更可能是从头发生的,预后较好。然而,由MDS引起的AML预后不良,常伴有5号和7号染色体的缺失。在化疗相关的急性髓系白血病中也可以发现类似的细胞遗传学。其余的AML亚型包括先前在FAB系统中定义的白血病,如AML和急性原巨核细胞白血病。
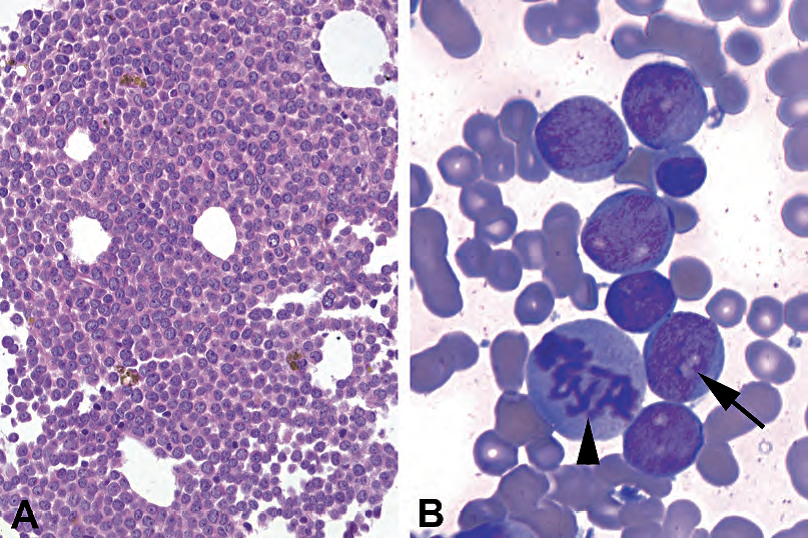
Figure 20.8. Acute myeloid leukemia. (A) The marrow biopsy material shows sheets of immature cells, with little or no background hematopoietic elements. Nucleoli appear dark on hematoxylin and eosin stain. (B) The aspirate shows clusters of myeloblasts with clear nucleoli (arrow). A large mitosis is visible (arrowhead); this in itself is not an unusual finding in the marrow.
图20.8 急性髓系白血病。(A)骨髓活检,示成片的未成熟细胞,很少或没有背景造血成分。HE染色显示核仁深染。(B)涂片显示成簇的原粒细胞,有透明核仁(箭)。可见巨大的核分裂象(箭头);这本身在骨髓中并不少见。
Table 20.1. Acute myeloid leukemia subtypes according to the old FAB and the newer WHO classifi cations.
表20.1。急性髓系白血病亚型,来自旧FAB和新WHO分类。
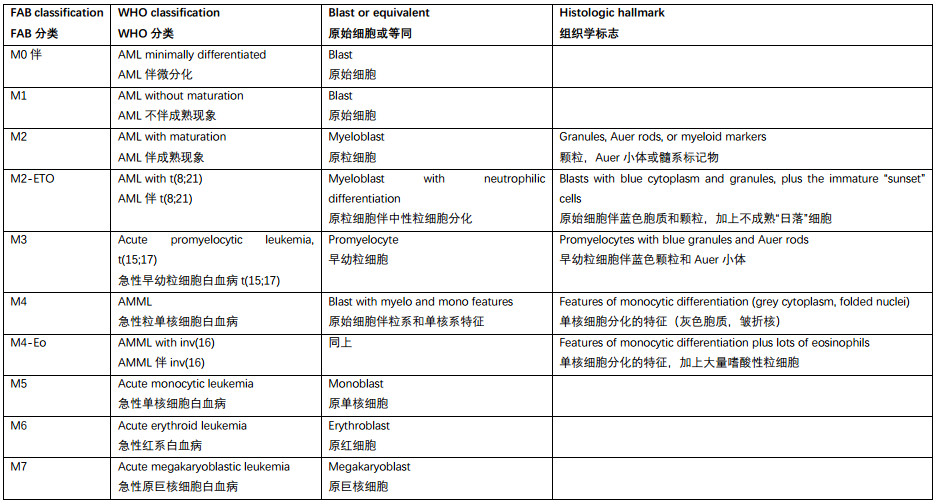
Note: AML, acute myeloid leukemia; AMML, acute myelomonocytic leukemia; eo, eosinophils.
注:AML,急性髓系白血病;急性粒单核细胞白血病;eo,嗜酸性粒细胞。
Histologically, acute myeloid leukemia usually presents as a hypercellular marrow mostly replaced by blasts. The differentiation of the blasts (and therefore the subclassification of the AML) is identified by morphology on the aspirate, flow cytometry, and cytogenetics. Some unique findings of the different subtypes include the following:
组织学上,急性髓系白血病通常表现为高细胞量的骨髓,大部分被原始细胞取代。通过涂片形态学、流式细胞术和细胞遗传学鉴定原始细胞的分化(以及AML的进一步分类)。不同亚型的一些独特发现包括:
t(8;21), acute myeloid leukemia–ETO: This subtype consists of a population of blasts with blue cytoplasm and granules, plus “sunset” cells, which are immature myeloid cells with salmon-pink granules, a pink cytoplasm with hof, and a peripheral blue rim. These look like a little sunset to some observers (Figure 20.9).
t(8;21)急性髓系白血病–ETO:具有蓝色胞质和颗粒的原始细胞,加上“日落”细胞。“日落”细胞是未成熟髓系细胞伴具有三文鱼红色颗粒,使胞质呈粉红色伴空晕和蓝色边缘,看起来有点像日落(图20.9)。
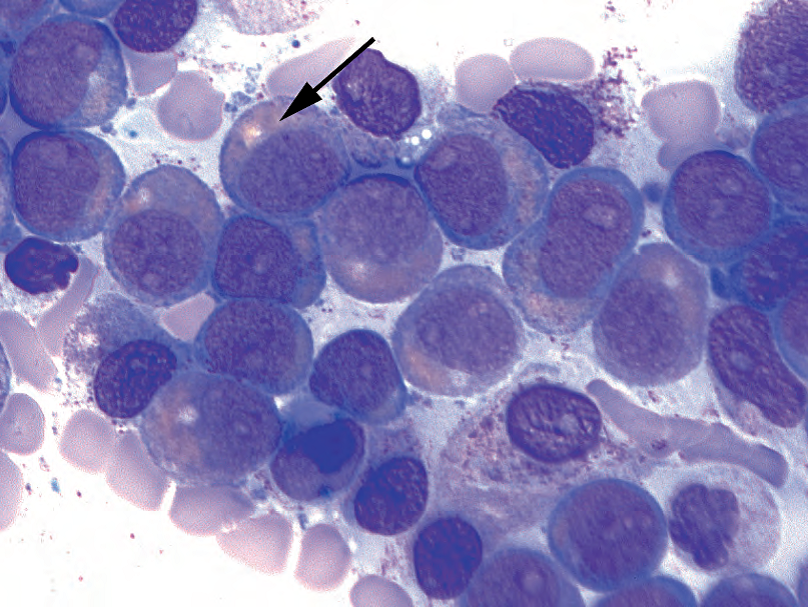
Figure 20.9. Acute myeloid leukemia–ETO. A population of the blasts have pink cytoplasm with pale hof, a peripheral blue rim, and pink granules (arrow).
图20.9 急性髓系白血病-ETO。母细胞群具有粉红色胞质和淡染空晕,周围有蓝色边缘和粉红色颗粒(箭)。
inv(16): This subtype is acute myeloid leukemia with both granulocytic and monocytic differentiation (monocytic differentiation is bluish grey cytoplasm and folded or convoluted nuclei) plus a high number of eosinophils in the marrow (Figure 20.10). Some of the eosinophils may have large abnormal blue granules (like basophils).
inv(16):兼有粒细胞和单核细胞分化(单核细胞分化为蓝灰色细胞质和折叠或卷曲的细胞核),加上骨髓中大量嗜酸性粒细胞(图20.10)。一些嗜酸性粒细胞可有大的异常的蓝色颗粒(像嗜碱性粒细胞)。
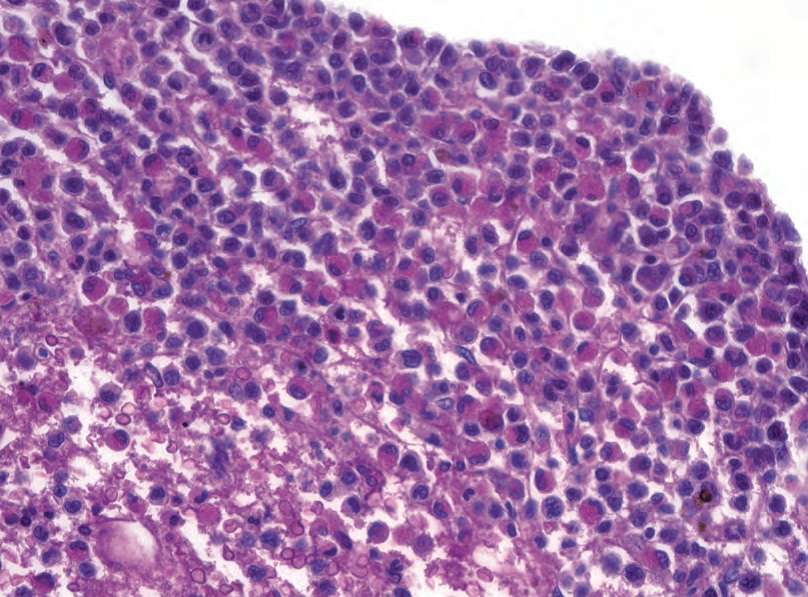
Figure 20.10. Acute myeloid leukemia inv (16). The marrow shows sheets of immature myeloid cells (the aspirate showed blasts) and numerous eosinophils.
图20.10 急性髓系白血病inv(16)。骨髓显示成片的未成熟髓样细胞(涂片显示原始细胞)和大量嗜酸性粒细胞。
t(15;17), acute promyelocytic leukemia: Technically there is not an increase in blasts but in promyelocytes. The nuclei are large with blast-like chromatin but folded (kidney-shaped), and the cytoplasm has large and numerous blue granules or Auer rods.
t(15;17)急性早幼粒细胞白血病:从技术上讲,并没有原始细胞增多,只是早幼粒细胞增多。核大,染色质呈母细胞样,但折叠(肾形),细胞质有大量蓝色大颗粒或Auer小体。
浆细胞异常(Plasma Cell Dyscrasias)
A normal marrow should have 1%–2% plasma cells, scattered in a perivascular distribution. Aggregates of plasma cells and atypical forms (large nucleoli, binucleate forms) are abnormal. The diagnosis of a plasma cell myeloma requires a marrow plasmacytosis with a monoclonal gammopathy. The marrow plasmacytosis is typically > 30% but can be as little as 10% if there are also lytic bone lesions or certain other criteria (see the WHO hematopathology book for the exact diagnostic criteria and variants). A softer call is the plasma cell dyscrasia, which implies that there is a plasma cell problem but does not meet the diagnostic criteria for myeloma. A localized plasma cell lesion without systemic gammopathy is a plasmacytoma.
正常骨髓应有1%-2%的浆细胞,在血管周围散在分布。浆细胞聚集和非典型浆细胞(大核仁、双核)是异常的。浆细胞骨髓瘤的诊断需要骨髓浆细胞增多伴单克隆丙种球蛋白病。骨髓浆细胞增多通常>30%,但如果同时存在溶骨性病变或某些其他标准,也可以低至10%(有关确切的诊断标准和亚型,参见WHO血液病理学分册)。更宽泛的说法是浆细胞异常,这意味着浆细胞有问题,但不符合骨髓瘤的诊断标准。无系统性丙种球蛋白病的局限性浆细胞病变是浆细胞瘤。
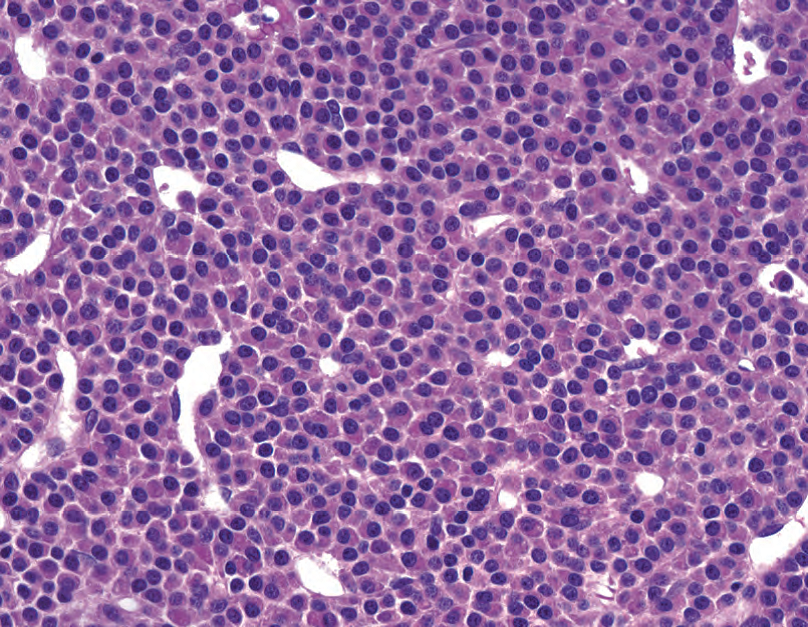
Figure 20.11. Myeloma. The marrow is replaced by sheets of plasma cells. Although the section is thick and the chromatin appears very dark, some nuclei show the distinct soccer-ball chromatin of plasma cells. The eccentric nucleus and abundant pink cytoplasm are also characteristic.
图20.11 骨髓瘤。骨髓被成片的浆细胞所替代。尽管切片厚,染色质似乎深染,但一些核显示浆细胞特有的足球样染色质。偏心核和丰富的粉红色细胞质也是其特征。
Sheets of plasma cells are recognizable on hematoxylin and eosin stain (Figure 20.11), but it is difficult to pick out a subtle interstitial plasmacytosis. CD138 can be used to help estimate the percentage. Immunostains for light chains kappa and lambda can identify an abnormally restricted (all kappa or all lambda) population, implying a monoclonal process. Flow cytometry tends to underestimate the number of plasma cells.
HE染色可辨认浆细胞片(图20.11),但很难分辨出细微的间质浆细胞增多。CD138可用于帮助估计百分比。κ和λ轻链的免疫染色可以识别异常的轻链限制性(全部κ或全部λ),这意味着单克隆性疾病。流式细胞术往往低估浆细胞的数量。
淋巴瘤(Lymphoma)
Lymphocytes in the bone marrow can be a normal or reactive finding. They can also be an indication of lymphoma involvement. History is important, as the marrow is an unlikely place for a presentation of occult lymphoma (i.e., without lymphadenopathy). However, non-Hodgkin lymphoma has a 30%–50% chance of involving the marrow at the time of diagnosis. The subtypes most likely to go to marrow are follicular, small lymphocytic lymphoma/chronic lymphocytic leukemia (SLL/CLL), mantle cell, lymphoblastic, Burkitt’s, and peripheral T-cell lymphomas. Diffuse large B cell is less likely.
骨髓中的淋巴细胞可测是正常的或反应性的,也可能提示淋巴瘤累及。病史很重要,因为骨髓不太可能出现隐匿性淋巴瘤(即没有淋巴结病)。然而,非霍奇金淋巴瘤在诊断时有30%-50%的机会累及骨髓。最有可能进入骨髓的亚型是滤泡型、小淋巴细胞淋巴瘤/慢性淋巴细胞白血病(SLL/CLL)、套细胞型、淋巴母细胞型、伯基特淋巴瘤和外周T细胞淋巴瘤。弥漫大B细胞不太可能。
Lymphoid infiltrates can come in four basic patterns:
淋巴浸润有四种基本类型:
Paratrabecular: This is a collection of lymphocytes that hugs the bony trabeculae. This pattern favors follicular lymphoma (Figure 20.12).

Figure 20.12. Paratrabecular aggregate. The arrow points to the center of this lymphoid aggregate, which appears more blue, relatively, than the surrounding marrow. One surface of the aggregate is plastered down to the bony trabeculum.
图20.12 小梁旁聚集灶。箭头指向淋巴聚集灶的中心,它比周围的骨髓更蓝。聚集灶的一面贴近骨小梁。
骨小梁旁:包裹骨小梁的淋巴细胞群。这种模式倾向于滤泡性淋巴瘤(图20.12)。
Nonparatrabecular: This is a lymphoid aggregate that is not closely associated with a trabeculum. Benign lymphoid aggregates (discussed further below) are common in elderly patients, but small lymphocytic and chronic lymphocytic lymphomas can also have this pattern (Figure 20.13).
非小梁旁:与小梁关系不密切的淋巴聚集灶。良性淋巴聚集灶(下文进一步讨论)常见于老年患者,但SLL/CLL也可能有这种模式(图20.13)。
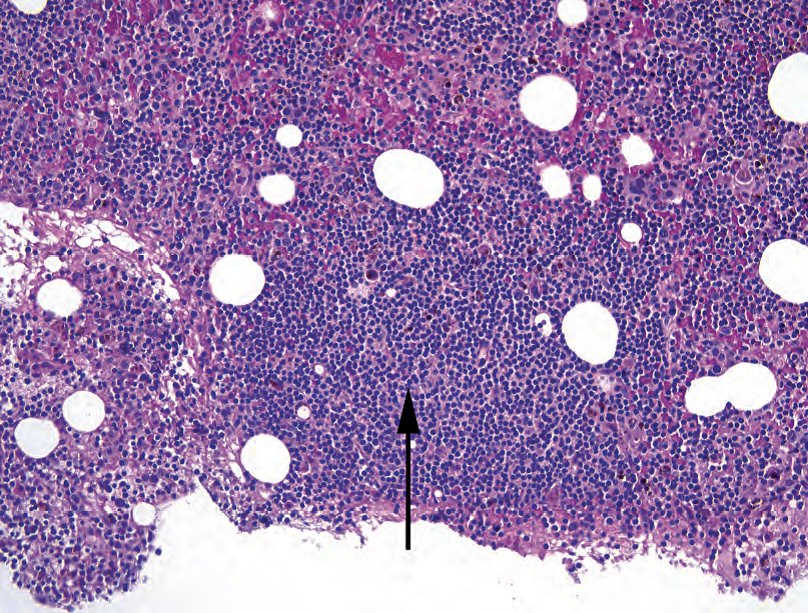
Figure 20.13. Nonparatrabecular aggregate in chronic lymphocytic leukemia. The arrow here points to the center of a free-floating, rounded lymphoid aggregate.
图20.13 慢性淋巴细胞白血病中的非小梁聚旁集。箭头指向自由漂浮的圆形淋巴聚集灶的中心。
Interstitial: This implies a scattered collection of lymphocytes in and among the marrow elements. It can be hard to pick out on H&E stain, because single lymphocytes will blend into the hematopoietic soup. Mantle cell and SLL/CLL tend to have this pattern, often in conjunction with nonparatrabecular aggregates.
间质性:淋巴细胞在骨髓成分内和骨髓成分之间散在聚集。HE染色很难分辨,因为单个淋巴细胞会混入造血细胞中。套细胞淋巴瘤和SLL/CLL往往具有这种模式,通常并存非旁小梁聚集灶。
Diffuse: This means sheets of lymphocytes replacing the marrow (Figure 20.14) and is more typical of aggressive lymphomas such as Burkitt’s lymphoma, diffuse large B-cell lymphoma, or advanced SLL/CLL.
弥漫性:这意味着大量淋巴细胞替代骨髓(图20.14),是侵袭性淋巴瘤较典型的表现,如伯基特淋巴瘤、弥漫大B细胞淋巴瘤或晚期SLL/CLL。

Figure 20.14. Diffuse large B-cell lymphoma in the marrow. The marrow is infiltrated by large atypical cells with prominent nucleoli, thick nuclear rims, abundant cytoplasm, and irregular nuclear membranes (arrow). This is suggestive of involvement by diffuse large B-cell lymphoma or carcinoma.
图20.14 骨髓中的弥漫大B细胞淋巴瘤。骨髓被大的非典型细胞浸润,核仁显著,厚的核环,细胞质丰富,核膜不规则(箭)。这种形态提示弥漫大B细胞淋巴瘤或癌。
Features of a benign lymphoid aggregate include a nonparatrabecular site; heterogeneous mixtures of lymphocytes, plasma cells, and histiocytes; well-demarcated borders; germinal centers; and older patient age. Immunostains can also help. A benign aggregate should be a mixture of B and T cells (CD20 and CD3). Beware the CD20 stain in a patient who is taking Rituximab, though, as this drug targets and eradicates CD20 expression. Use another B-cell marker such as CD22, CD79a, or PAX5.
良性淋巴聚集灶的特征包括非小梁旁部位;淋巴细胞、浆细胞和组织细胞形成的异质性混合物;边界清楚;生发中心;患者年龄较大。免疫染色也有帮助。良性聚集灶应该是B细胞和T细胞(CD20和CD3)的混合物。当心正在服用利妥昔单抗的患者的CD20染色,这种药物靶向并消除CD20的表达。可用其他B细胞标记物,如CD22、CD79a或PAX5。
Hodgkin’s lymphoma in the marrow can be extremely subtle, as the defining trait of Hodgkin’s is a mixed infiltrate with scattered neoplastic (Reed-Sternberg) cells. Focal fibrosis or granulomatous inflammation may be all that is seen initially; immunostains can often pick out the rare neoplastic cells.
骨髓中的霍奇金淋巴瘤可能非常微妙,因为霍奇金淋巴瘤的特征是散在的肿瘤细胞(Reed-Sternberg)的混合性浸润。最初可能只看到局灶性纤维化或肉芽肿性炎症;免疫染色常常能显示罕见的肿瘤细胞。
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。
本站欢迎原创文章投稿,来稿一经采用稿酬从优,投稿邮箱tougao@ipathology.com.cn
相关阅读
 数据加载中
数据加载中
我要评论

热点导读
-

淋巴瘤诊断中CD30检测那些事(五)
强子 华夏病理2022-06-02 -

【以例学病】肺结节状淋巴组织增生
华夏病理 华夏病理2022-05-31 -

这不是演习-一例穿刺活检的艰难诊断路
强子 华夏病理2022-05-26 -

黏液性血性胸水一例技术处理及诊断经验分享
华夏病理 华夏病理2022-05-25 -

中老年女性,怎么突发喘气困难?低度恶性纤维/肌纤维母细胞性肉瘤一例
华夏病理 华夏病理2022-05-07






共0条评论