[导读] 编译整理:Abin
第3章 感染和炎症
(Infection and Inflammation)
Let us review the types of inflammatory responses you may see. It seems very basic, but learning to differentiate inflammatory changes from dysplastic ones is a fundamental goal in pathology training.
先复习一下,你可能会看到的炎症反应类型。这似乎非常基础,但学会区分炎症改变和异型增生改变是病理学培训的基本目标。
3.1急性(Acute)
Acute changes are the result of recent tissue damage, either from trauma, ischemia, toxins, or infection. Features include the following:
急性炎症改变是近期组织损伤的结果,病因包括创伤、缺血、毒素和感染,等。其特点包括:
l Vascular congestion
l 血管充血()
l Edema
l 水肿()
l Fibrinous exudate
l 纤维素性渗出物()
l Tissue damage and/or necrosis
l 组织损伤和/或坏死()
l Neutrophils (“purulence”, polymorphonuclear leukocytes, polys
l 中性粒细胞(“化脓性”,多形核白细胞,简写polys)())
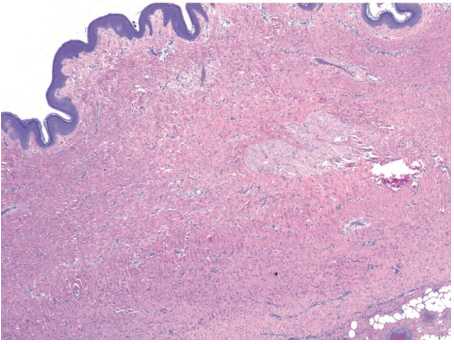
Acute inflammation can be followed by resolution (healing), fibrosis or scar, abscess formation (Figure 3.1), or a chronic inflammatory stage. Evidence of recent damage and reparative changes includes granulation tissue, hemosiderin, lipid-laden macrophages, and fibroblast proliferation.
急性炎症后可以消退(愈合)、纤维化或形成瘢痕、脓肿(图3.1),或转变成慢性炎症。近期损伤和修复性改变的证据包括肉芽组织、含铁血黄素、富含脂质的巨噬细胞和纤维母细胞增殖。
(译注:注意比较proliferation增殖与hyperplasia增生。fibroblast纤维母细胞或成纤维细胞)
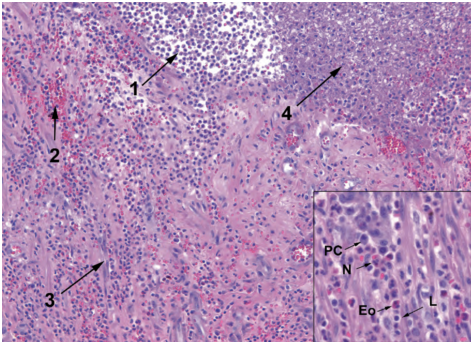
Figure 3.1 Acute inflammation and abscess formation. This example of the acute inflammatory response shows collections of neutrophils (abscess formation, 1), extravasated blood (2), prominent capillaries (3), and fibrin accumulation (4). Inset: the mixed inflammatory infiltrate includes plasma cells (PC), neutrophils (N), eosinophils (Eo), and lymphocytes (L).
图3.1 急性炎症和脓肿形成。这例急性炎症反应显示中性粒细胞聚集(脓肿形成,1)、渗出的血液(2)、显著的毛细血管(3)和纤维素积聚(4)。插图:混合性炎症细胞浸润,包括浆细胞(PC)、中性粒细胞(N)、嗜酸性粒细胞(Eo)和淋巴细胞(L)。
Granulation tissue has a characteristic look of a watery or myxoid background with sparse fibroblasts floating in it and a proliferation of inflammatory cells (all types) and capillaries (Figure 3.2). The endothelial cells of the capillaries can become quite prominent.
肉芽组织具有特征性表现:水样或粘液样背景,稀疏的纤维母细胞漂浮在其中,炎症细胞(所有类型)和毛细血管增殖(图3.2)。毛细血管的内皮细胞可以变得非常显著。
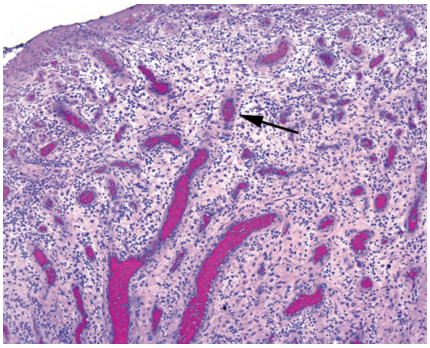
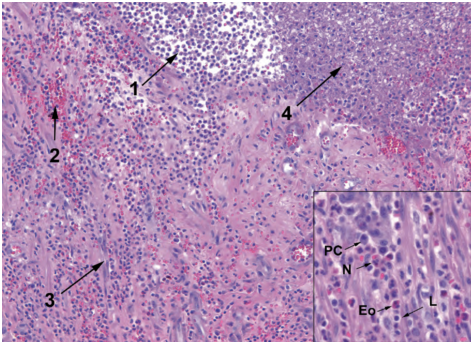
Figure 3.2 Granulation tissue is characterized by a loose myxoid background with fibroblasts and inflammatory cells and by prominent capillaries with plump endothelial cells and thick walls. The stroma appears condensed and thickened around the capillaries, giving them a pink halo (arrow).
图3.2 肉芽组织的特征:疏松的黏液样背景,纤维母细胞和炎症细胞,显著的毛细血管伴有丰满的内皮细胞和厚的血管壁。围绕在毛细血管周围的间质显得浓缩和增厚,形成粉红色光环(箭号)。
(译注:halo(绘画等中环绕圣人头上的)光环,光轮)
Biopsy site changes, a term often used to indicate evidence of a recent procedure, include fibroblast proliferation (early scar), foreign body–type giant cells, suture material, foamy macrophages, fat necrosis, and inflammation. They have a more solid look to them than granulation tissue (Figure 3.3).
活检部位改变,这个术语常用于描述近期手术证据,包括纤维母细胞增殖(早期瘢痕)、异物型巨细胞、缝合材料、泡沫状巨噬细胞、脂肪坏死和炎症。与肉芽组织相比,它们看起来更加实性(图3.3)。
(译注:solid,坚实的,实性,实体。大体描述一种质地较硬但不到坚硬的程度,如,实性肿瘤/非实性肿瘤(白血病)。镜下描述细胞较丰富,结构较紧凑,非囊性)
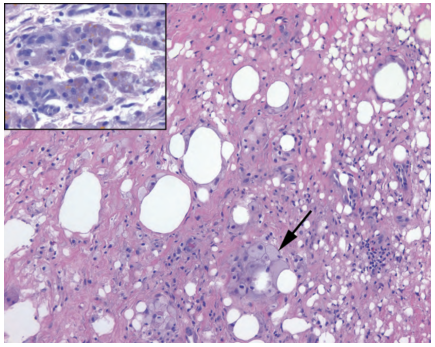
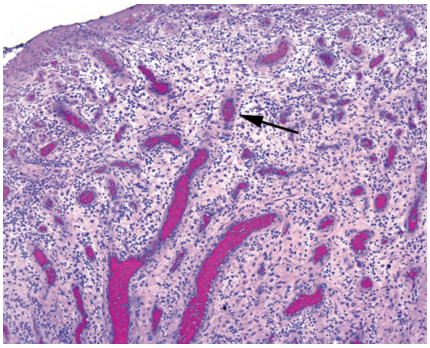
Figure 3.3 Biopsy site changes. In this subcutaneous specimen, collagen has replaced most of the fat cells, and foamy histiocytes can be seen ingesting some residual fat (arrow). Inset: Hemosiderin in macrophages (golden yellow to brown granules) can be seen in sites of prior trauma or bleeding.
图3.3 活检部位改变。这是皮下组织的标本,胶原蛋白已经取代了大部分脂肪细胞,可以看到泡沫状组织细胞摄取了一些残留的脂肪(箭号)。插图:在先前的创伤或出血部位可以看到巨噬细胞中的含铁血黄素(金黄色至棕色颗粒)。
Scar tissue implies that a dense thick collagen has replaced the normal structures. In the skin, a dermal scar is evidenced by a homogeneous pink layer of collagen and absence of adnexal structures (Figure 3.4).
瘢痕组织是指一种致密的厚胶原已经取代了正常的结构。在皮肤中,瘢痕表现为一层均匀的粉红色胶原,没有附属器结构(图3.4)。
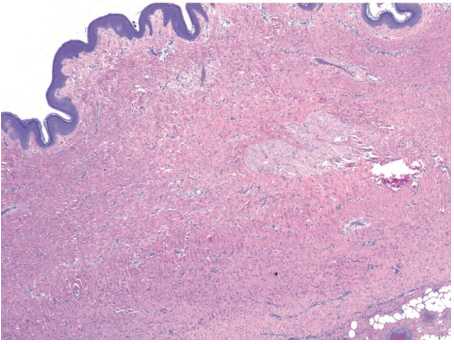
Figure 3.4 Dermal scar. Dense pink collagen has replaced the adnexal structures and displaced the subcutaneous fat in this biopsy site.
图3.4 皮肤瘢痕。致密的粉红色胶原已经取代了附属器结构,并取代了活检部位的皮下脂肪。
3.2慢性(Chronic)
Chronic changes are the result of repetitive or sustained tissue damage due to trauma, ischemia, toxins, infection, or autoimmune processes. Features include the following:
慢性炎症改变是由于创伤、缺血、毒素、感染或自身免疫疾病引起的重复性或持续性组织损伤的结果。其特点包括:
l Increased vascularity and/or fibrosis (attempts to heal
l 血管增多和/或纤维化(试图愈合)())
l Tissue destruction
l 组织破坏()
l Lymphocytes, macrophages, plasma cells, eosinophils
l 淋巴细胞、巨噬细胞、浆细胞、嗜酸性粒细胞()
What is a macrophage? The precursor is a circulating monocyte, part of the myeloid lineage of blood cells (myeloid generally refers to cells in the granulocyte and monocyte groups, although it can also mean all cells that mature in the bone marrow, i.e., the opposite of lymphoid). The monocyte leaves the circulation and becomes a tissue macrophage. It can differentiate into organ-specific resident macrophages, such as microglia, Kupffer cells, and alveolar macrophages. It can also go to an area of inflammation and become activated, participating in the immune response. Activated macrophages are also called histiocytes and may be “epithelioid,” as in a granuloma, or “foamy,” as in lipid-laden or xanthomatous. Finally, macrophages can acquire multiple nuclei to become a Langerhans giant cell (ring of nuclei) or a foreign body–type giant cell (scattered nuclei).
什么是巨噬细胞?其前体是血液循环中的单核细胞,是血细胞中髓系细胞的一部分(髓系通常指粒细胞群和单核细胞群中的细胞,但髓系也可以指在骨髓中成熟的所有细胞,即,相对于淋巴细胞系)。单核细胞离开循环,成为组织巨噬细胞。它可以分化为器官特异性常驻巨噬细胞,如小胶质细胞、库弗细胞和肺泡巨噬细胞。它也可以进入炎症区域并被激活,参与免疫反应。活化的巨噬细胞也称为组织细胞,可能呈“上皮样”,如肉芽肿;也可能呈“泡沫状”,如富含脂质的组织细胞或黄色瘤中的组织细胞。最后,巨噬细胞可以形成多核,形成朗格汉斯巨细胞(核排列成环形)或异物型巨细胞(核散在分布)。
(译注:注意原文笔误,多核组织细胞或多核巨细胞应为Langhans(朗罕)巨细胞,而Langerhans(郎格汉斯)细胞是一种树突状细胞,功能上属于抗原提呈细胞)
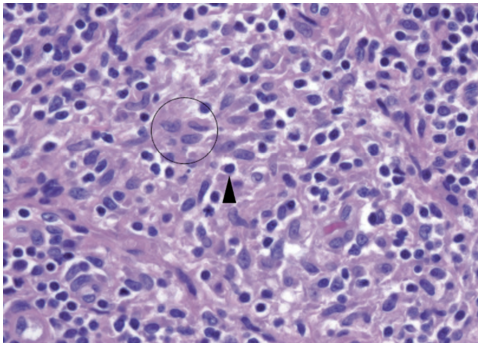
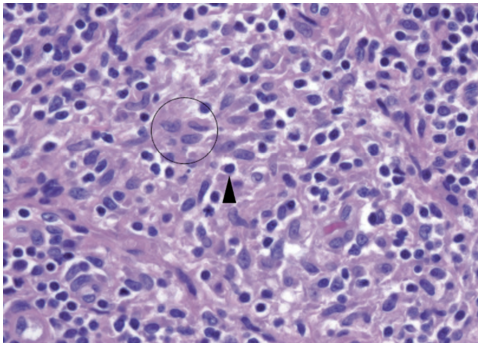
Figure 3.5 Histiocytes appear as pale folded nuclei within an area of inflammation; the cell borders are indistinct, but the nuclei are surrounded by light pink cytoplasm (circle). Compare the pale chromatin to that of the neighboring lymphocyte (arrowhead).
图3.5 组织细胞在炎症区域内表现为淡染的折叠细胞核;细胞边界模糊,但细胞核被淡粉色细胞质包围(圆圈)。将淡染的染色质与相邻淋巴细胞(箭头)的染色质进行比较。
Histologically, histiocytes have a bland and fade-into-the-background look to match their name (literally, “tissue cell”). They have pale-pink granular cytoplasm, sometimes with chunky phagocytosed bits of material, and indistinct cell borders (Figure 3.5). The nuclei are light with crisp outlines, oval in shape, and often grooved. In tissue, a collection of histiocytes appears as an ill-defined pink area that is easy to miss. The nuclei often stream in a circular pattern like fish swimming in a barrel. Foamy macrophages are stuffed with lipid debris or organisms, and can have an almost signet-ring appearance.
组织学上,组织细胞的形态学温和,淡入背景,很匹配其名称(字面意思就是“组织细胞”)。它们有淡粉色颗粒性细胞质,有时有大块被吞噬的物质,细胞边界模糊(图3.5)。细胞核较淡,轮廓清晰,呈椭圆形,常有凹槽。在组织中,组织细胞的聚集表现为一个界限不清的粉红色区域,很容易被忽略。细胞核通常呈环形流动,就像鱼在桶中游泳一样。泡沫状巨噬细胞内充满脂质碎片或微生物,可能很像印戒样外观。
What are eosinophils? Eosinophils have a bilobed nucleus and big red granules. They are usually an indication of an immune/IgE response, such as to drug allergy or parasites.
什么是嗜酸性粒细胞?嗜酸性粒细胞有双叶核和大的红色颗粒。它们通常提示免疫反应/IgE反应,例如药物过敏或寄生虫。
We usually refer to the presence of lymphocytes as chronic inflammation. Lymphocytes plus neutrophils equals acute and chronic inflammation. In the gastrointestinal tract, instead of acute we use active, such as active chronic gastritis or active chronic inflammatory bowel disease. Inactive in the gastrointestinal tract means increased lymphocytes but no polys.
我们通常将存在淋巴细胞的炎症称为慢性炎症。淋巴细胞加中性粒细胞等于急性和慢性炎症。在胃肠道中,我们不称为急性,而是称为活动性,如活动性慢性胃炎或活动性慢性炎症性肠病。胃肠道内非活动性炎症是指淋巴细胞增多,但中性粒细胞不增多。
3.3肉芽肿性(Granulomatous)
A granulomatous appearance indicates a specific type of chronic inflammation with a small differential; it can be a result of mycobacteria (plus a few other bacteria), fungal infection, autoimmune disease, some toxins or irritants, and sarcoid. Granulomas are divided into caseating (usually infectious) and noncaseating.
肉芽肿性形态提示一种特殊类型的慢性炎症,但差别不大;它可能是由分枝杆菌(加上其他几种细菌)、真菌感染、自身免疫性疾病、某些毒素或刺激物以及结节病引起的。肉芽肿分为干酪样(通常为感染性)和非干酪样。
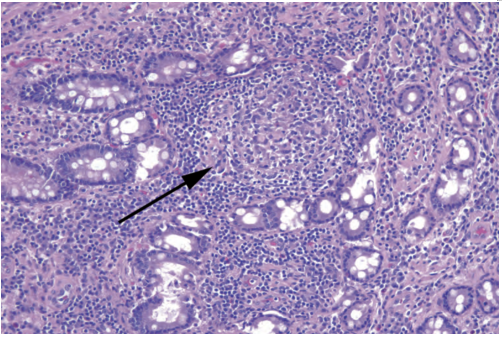
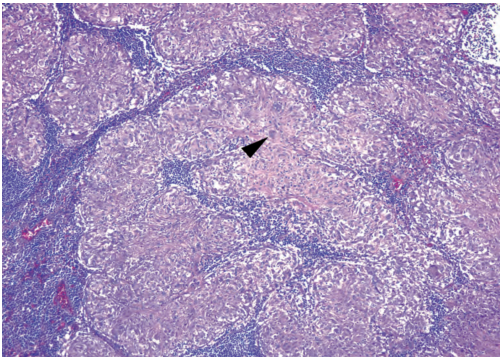
The histologic appearance of a granuloma is a microscopic aggregate of histiocytes, with surrounding lymphocytes and plasma cells. The appearance ranges from tiny collections of histiocytes (as in Crohn’s disease; Figure 3.6), to large well-circumscribed whorls of cells (sarcoid; Figure 3.7), to a layer of histiocytes surrounding a pool of caseous necrosis (tuberculosis, fungus; Figure 3.8). Giant cells are helpful but not essential. Old granulomas can become hyalinized and acellular (Figure 3.9).
肉芽肿的组织学表现为组织细胞的显微镜下聚集,周围有淋巴细胞和浆细胞。范围从微小的组织细胞聚集(如克罗恩病;图3.6),到边界清晰的旋涡状细胞聚集(结节病;图3.7),再到一层组织细胞围绕着干酪样坏死池(结核、真菌;图3.8)。巨细胞有助于识别,但不是必需的。陈旧性肉芽肿可能变得透明和无细胞(图3.9)。
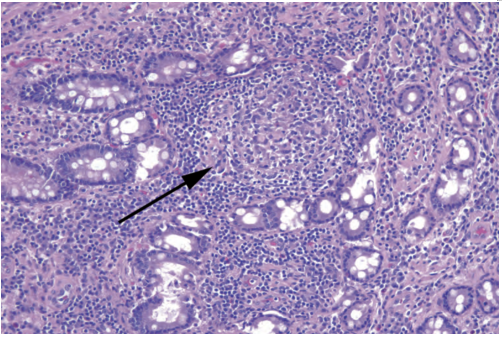
Figure 3.6 Granulomas in Crohn’s disease. These granulomas of the colon are subtle (arrow), and the pale histiocytes may be seen only on high power. A surrounding collar of lymphocytes is common.
图3.6 克罗恩病的肉芽肿。结肠的这些肉芽肿很轻微(箭号),只有在高倍镜下才能看到淡染的组织细胞。周围常见衣领状淋巴细胞围绕。
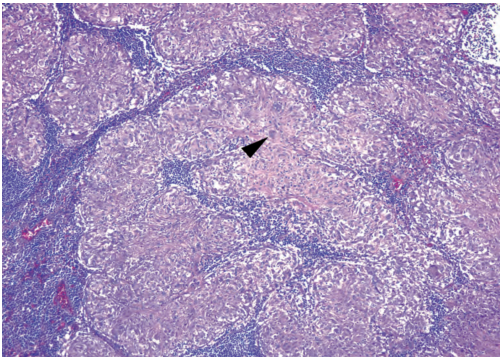
Figure 3.7 Granulomas in sarcoid. These granulomas are often more substantial and more easily recognized than those in Crohn’s disease. They appear as well-defined masses of pink histiocytes. Occasional multinucleated giant cells (arrowhead) are present.
图3.7 结节病的肉芽肿。与克罗恩病的肉芽肿相比,这些肉芽肿通常更明显,更容易识别。它们表现为边界清晰的粉红色组织细胞团块。偶尔出现多核巨细胞(箭头)。
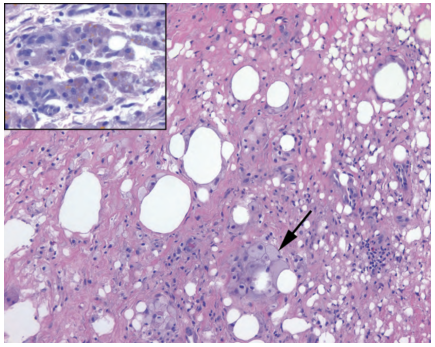
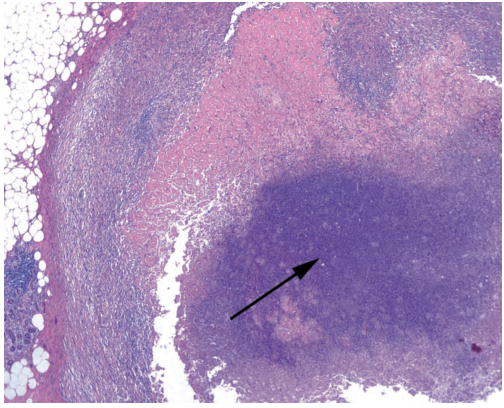
Figure 3.8 Caseating granulomas in tuberculosis. The histiocytes in these granulomas are visible only at the periphery, as the center is a mass of necrosis and cellular debris (arrow).
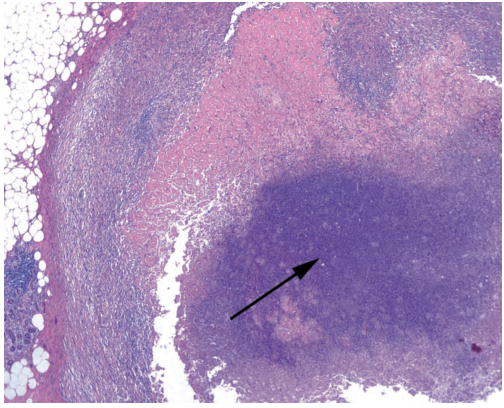
图3.8 结核中的干酪样肉芽肿。这些肉芽肿中的组织细胞仅在周围可见,因为中心是一团坏死和细胞碎片(箭号)。
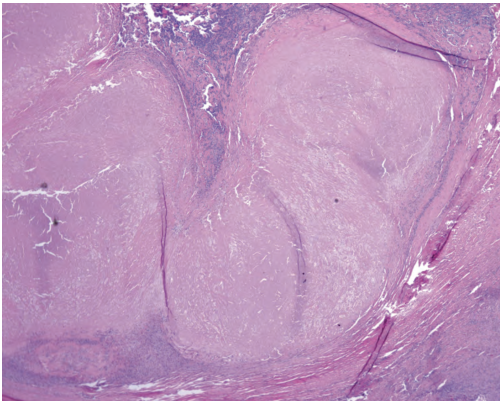
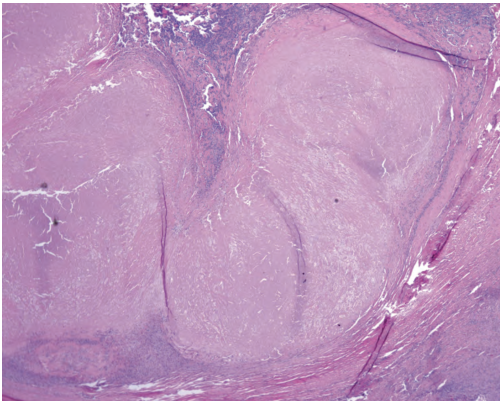
Figure 3.9 Hyalinized granuloma. The amorphous area of hyalinized collagen likely represents old, burned-out necrosis.
图3.9 玻璃样变的肉芽肿。透明变性的胶原形成无定形区域,可能代表陈旧性、燃烬的坏死。
未完待续
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。












共0条评论