外科病理学实践:诊断过程的初学者指南 | 第4章 复杂上皮的解读
第4章 复杂上皮的解读(Interpreting the Complex Epithelium)
Complex, or multilayered, epithelia (squamous and urothelial) may progress through a spectrum of changes, from benign hyperplasia and/or metaplasia, to inflamed reactive atypia, to dysplasia, to carcinoma in situ (CIS), to invasive carcinoma (crossing the basement membrane). The progression is not inevitable or consistent, and some lesions will regress. However, true dysplasia is generally regarded as a premalignant condition. Carcinoma in situ is one step from invasive cancer and therefore treated aggressively. Some lesions are easily monitored clinically, such as those in the cervix and oral cavity, and therefore each phase of change can be seen, biopsied, and followed. Others, such as in the nasopharynx, are generally not noticed until they are fairly large and/or symptomatic. This chapter will touch on basic principles that these epithelial layers have in common and introduce some organ systems that are covered in greater detail later in the book.
复杂或多层上皮(鳞状上皮和尿路上皮)可能通过一系列形态学改变的谱系而发生进展,从良性增生和/或化生,到炎症反应性非典型增生,到异型增生,到原位癌(CIS),再到浸润性癌(穿过基底膜)。进展并非不可避免、必然发生的,也不是持续不变、一直向前的,有些病变会消退。然而,一般认为真正的异型增生是癌前状态。原位癌是浸润性癌的前一步,因此需要积极治疗。有些病变在临床上很容易监测,例如宫颈和口腔,因此每个改变阶段都可以看到、活检和随访。其他部位,如鼻咽,通常在相当大和/或有症状之前不会被发现。本章将涉及这些复层上皮的共同的基本原理,并介绍一些器官系统,这些系统将在本书后面的章节中详细介绍。
(译注:关于形态学“谱系”,一般是指连续的或不连续的有限的变化范围。变化范围有两个极端,以鳞癌发生发展的形态学改变为例,一端为反应性增生,另一端为浸润性鳞癌。当然,谱系之外还有一些形态学表现,如,正常组织学不在该谱系之中,鳞癌充分形成后再发生的间变也不在其中。
关于非典型性(atypia)和异型性(dysplasia)。大多数观点认为,atypia只是单纯的形态学描述,不是良性或恶性的定性术语,它不加区分地包括良性反应性改变和肿瘤性形态学改变。而dysplasia专指肿瘤性形态学改变。在不同语境中,特别是在不规范的简称中,atypia也可译为非典型增生,dysplasia也可译为异型增生)
上皮解读方法:一般原则(Approach to the Epithelium: General Principles)
On low power (4×), look for the following:
在低倍镜(4×)下,有意识地观察以下各项:
Type of epithelium: Is it squamous, columnar, ciliated?
上皮类型:鳞状、柱状、纤毛状?
Architecture: Is it an exophytic structure, such as a verrucous lesion or a papilloma? Is there downward growth, as in an inverted papilloma or invasive lesion?
结构:是外生结构吗?如疣状病变或乳头状瘤?有向下生长吗?如内翻性乳头状瘤或浸润性病变?
Keratinization: Is keratinization present or absent? Hyperkeratosis? Parakeratosis? Mounds or church spires of keratin (as in a wart)?
角化:有无角化?角化过度?角化不全?角化物形成的丘或教堂尖顶(如疣)?
Thickness of the epithelium: Is the epithelium thickened and irregular (acanthotic) or thin and flat (atrophic)? A markedly thickened epithelium may indicate irritation and hyperplasia but not necessarily dysplasia.
上皮厚度:上皮是增厚且不规则(棘皮症或棘层肥厚)?还是薄而扁平(萎缩)?上皮明显增厚可能表明刺激和增生,但不一定是异型增生。
Architectural orderliness: Is there a clear difference between the basal layer and the superficial layer? Are the rows of cells orderly (Figure 4.1)? Are the nuclei lined up, either parallel to the surface or perpendicular to it?
结构规则有序:底层和表层之间有明显的区别吗?每行细胞是否排列有序(图4.1)?核是否排列成行,是平行于表面还是垂直于表面排列的?
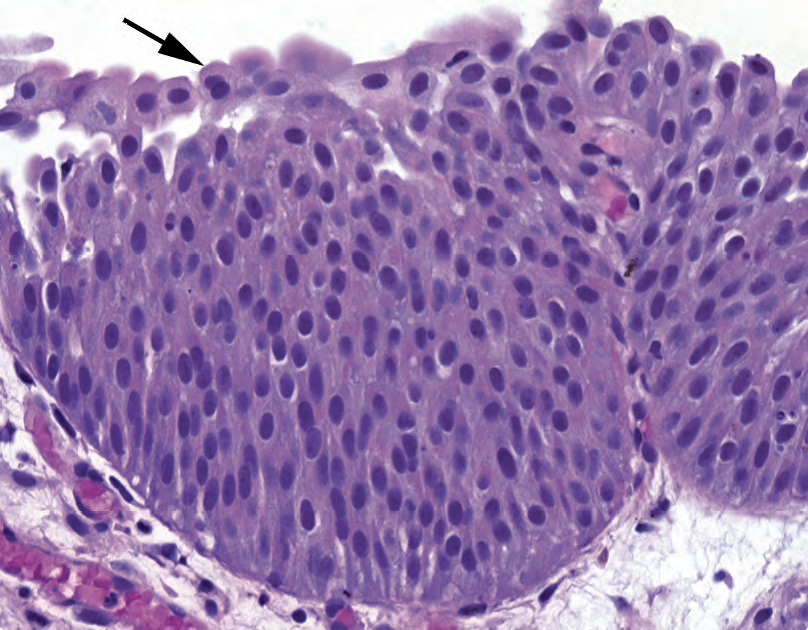
Figure 4.1. Polarity in an epithelium. In this section of urothelium, although it is thickened relative to normal, all of the nuclei can be seen to be roughly perpendicular to the surface; they “know which way is up.” Plump umbrella cells are visible at the surface (arrow).
图4.1。上皮的极性。在这一段尿路上皮中,尽管比正常尿路上皮相对增厚,但可以看到所有的细胞核大致垂直于表面;它们“知道哪条路是向上的。”在表面可以看到丰满的伞细胞(箭头)。
General color: What color is it? Although it is hard to compare one slide to another, within a single slide differences in color can make a dysplastic or inflamed area stand out as dark or blue. Islands of bright pink, on the other hand, may indicate deep keratinization, which is a feature of invasion.
一般颜色:什么颜色?虽然很难将一张切片与另一张切片进行比较,但在一张切片中,颜色的差异会使异型增生或炎症区域显得更加明显,呈黑色或蓝色。另一方面,明亮的粉红色的岛状物可能提示深部角化,这是浸润的特征。
On high power, look for the following:
在高倍镜下,有意识地观察以下各项:
Architectural orderliness and polarity: Try to find a well-oriented fragment, not a tangential cut. In a benign, even reactive epithelium, all of the nuclei should appear to “know which way is up.”
结构规则和极性:试着找到切面方向良好的片段,而不是斜切面。在良性、甚至是反应性上皮中,所有的细胞核似乎都“知道向上的方向”
(译注:关于正确的切面。以切黄瓜为例,纵切得长条形,横切或垂直切面得圆形,沿切线方向或斜切得椭圆形或一块皮)
Mitotic figures: Although a few mitoses near the basal layer are acceptable, mitoses higher in the epithelium are not. As above, a well-oriented fragment is very helpful.
核分裂象:虽然基底层附近有少量核分裂是可以接受的,但上皮细胞中更高的部位出现核分裂不是正常现象。如上所述,观察切面方向良好的片段,非常有用。
(译注:关于核分裂象的位置。正常鳞状上皮基底层核分裂象,基底层上方2~3层细胞可以出现核分裂象)
Dyskeratotic cells: Small, intensely pink, shriveled round cells that have detached from their neighbors (Figure 4.2) can be a feature of dysplasia.
角化不良细胞:小的、深染粉红色的、皱缩的圆形细胞从邻近细胞分离(图4.2),可能是异型增生的一个特征。
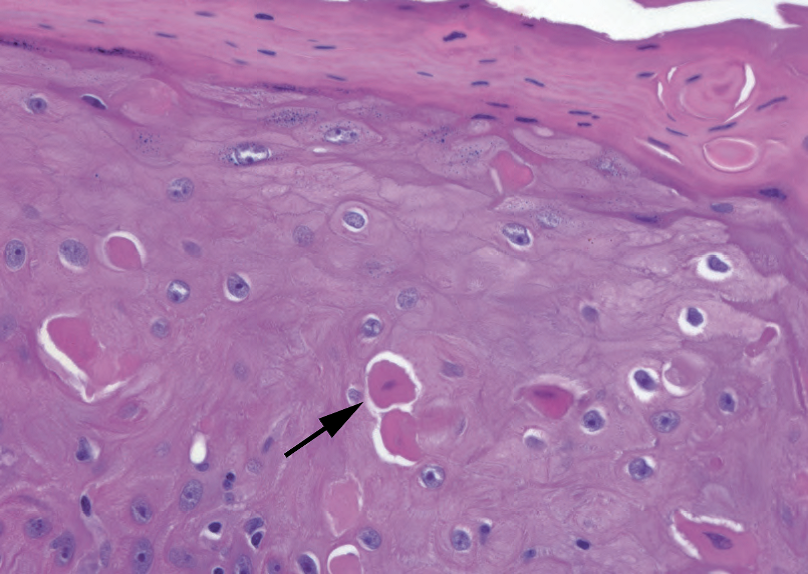
Figure 4.2. Dyskeratotic cells in the epidermis. These cells are essentially mummified; their nuclei are dying, and they have lost their connections to other cells. Their dense pink keratin stands out relative to the neighboring cells (arrow).
图4.2。表皮角化不良细胞。核正在经历死亡,这些细胞基本上是干尸化的,与邻近细胞已经失去联系。它们的深染粉红色角蛋白比邻近细胞更明显(箭头)。
Inflammation: Look for polymorphonuclear leukocytes (polys), plasma cells, and lymphocytes. Keep a high threshold for dysplasia in the setting of intense acute inflammation (polys).
炎症:寻找中性粒细胞、浆细胞和淋巴细胞。在剧烈急性炎症背景下,保持异型增生的高阈值(即,不要轻易诊断异型增生)。
Nuclei, eggs versus boulders (Figure 4.3): Reactive nuclei may enlarge but stay smooth and round to oval, and their chromatin condenses into several small nucleoli or speckles, like a bird’s egg. The chromatin may have an overall grey-blue look, and the nuclear membrane is often indistinct. Dysplastic or immature nuclei, however, appear to have too much chromatin. They are large and tend to be angulated with irregular nuclear membranes (like boulders), and the chromatin is uniformly dense and dark, almost like it was drawn with charcoal. Nuclear membranes may also appear thicker and more prominent.
核、蛋与大圆石(图4.3):反应性细胞核可能扩大,但保持轮廓光滑的圆形至椭圆形,其染色质浓缩成几个小碎核或斑点,如鸟蛋。染色质整体上呈灰蓝色,核膜通常不明显。然而,异型增生或未成熟的细胞核似乎有过多的染色质。核大,往往因不规则的核膜而成角(像是大圆石),染色质均匀致密,深染,几乎像是用木炭画出来的。核膜也可能显得更厚、更明显。
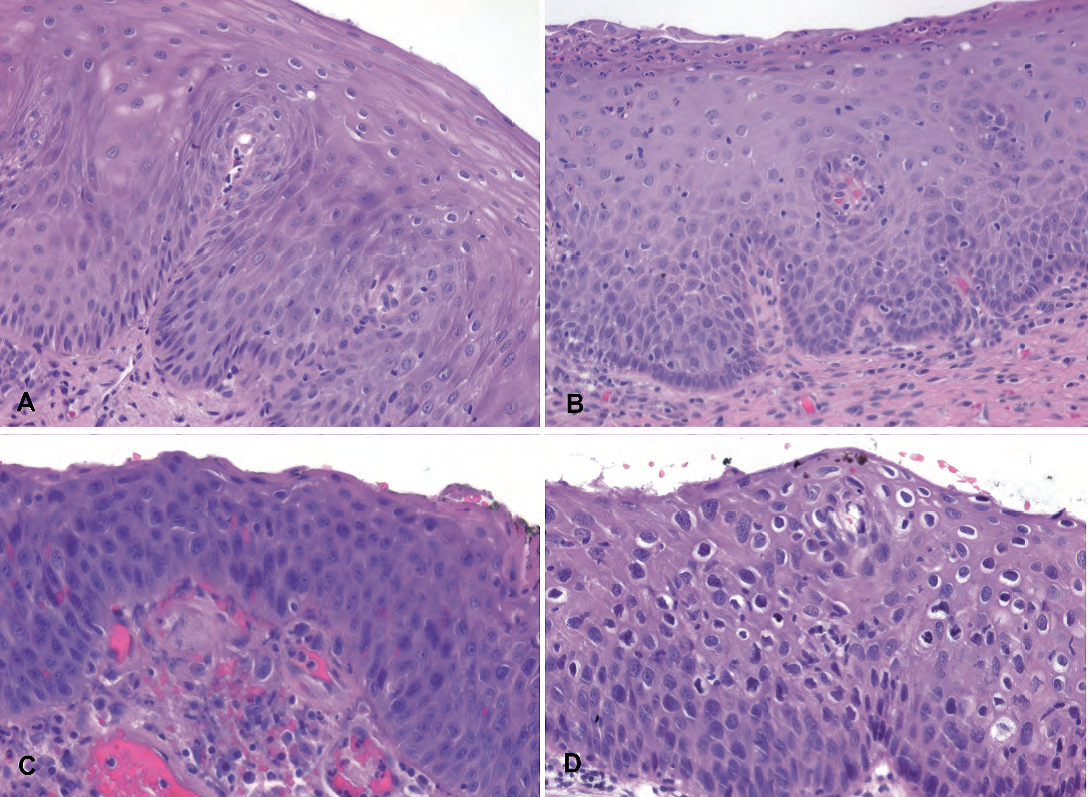
Figure 4.3. Examples of reactive, benign nuclei (A, B) and dysplastic nuclei (C, D). In reactive conditions, the nuclei may be enlarged and have visible nucleoli, but the N/C ratios are still low (abundant cytoplasm), there is nuclear polarity relative to the surface, the chromatin is not too dark, and the nuclear membranes are smooth and oval. Maturation is visible in that as cells get closer to the surface the nuclei get smaller and the cytoplasm more abundant. In dysplasia, the nuclei are significantly darker, the N/C ratios are higher, there is more disorder to the epithelium, and the nuclei (being more closely packed) may take on irregular shapes to fit more closely together, similar to boulders in a rock wall.
图4.3。反应性、良性细胞核(A、B)和异型增生细胞核(C、D)。在反应性情况下,核可能扩大,可见核仁,但N/C比仍然低(细胞质丰富),相对于表面存在核极性,染色质不太深染,核膜光滑、椭圆形。可见成熟现象,表现为接近表面的细胞核变小,细胞质更丰富。在异型增生中,细胞核明显更深染,N/C比较高,更不规则,细胞核(排列更紧密)可能呈现不规则形状,以更紧密地嵌合在一起,类似于石墙中的大圆石。
Nucleoli: Prominent nucleoli are actually a feature more suggestive of reactive changes than of dysplasia. A prominent nucleolus in a background of fine pale chromatin, in a smoothly rounded nucleus, is likely benign. Carcinomas usually do not acquire large dark nucleoli until they become invasive.
核仁:明显核仁实际上更提示反应性改变的特征,而不是异型增生。在平滑圆形的细胞核中,在细腻淡染的染色质背景中,明显核仁可能是良性的。在浸润之前,癌通常不会获得大的深染核仁。
Nuclear to cytoplasmic (N/C) ratios: The N/C ratio is normally high in the basal layer but should fall off as the cells mature. A high N/C ratio at the surface, especially in the setting of “boulder” nuclei, is very worrisome. This creates the impression of blueness at low power.
细胞核与细胞质(N/C)的比例:正常情况下,基底层N/C比高,但随着细胞成熟,N/C比应下降。表面的高N/C比,特别是在“大圆石”核的情况下,是非常令人担忧的。这会在低倍镜下产生蓝色的印象。
Invasion: Stromal invasion is a sure sign of cancer but is not always obvious. Pseudoepithe-liomatous hyperplasia and tangential sectioning are the main mimickers. Features that suggest true invasion include deep aberrant keratinization (pinking up) and single infiltrating cells with atypical nuclei (Figure 4.4). The basement membrane border should appear ragged and discontinuous in invasion. Well-differentiated squamous cell carcinoma can acquire prominent nuclei (usually not seen in CIS) and mimic reactive nuclei, but it should have the architectural features of invasion.
浸润:间质浸润是癌的必然迹象,但并不总是明显的。假上皮瘤样增生和斜向切片是主要的假冒现象。提示真正浸润的特征包括深部异常角化(变得更红)和单个浸润细胞伴异型性癌(图4.4)。基底膜边界在侵入时应呈现参差不齐和不连续。高分化鳞状细胞癌可以获得明显的细胞核(通常在CIS中不可见)和貌似反应性细胞核,但它应该具有浸润的结构特征。
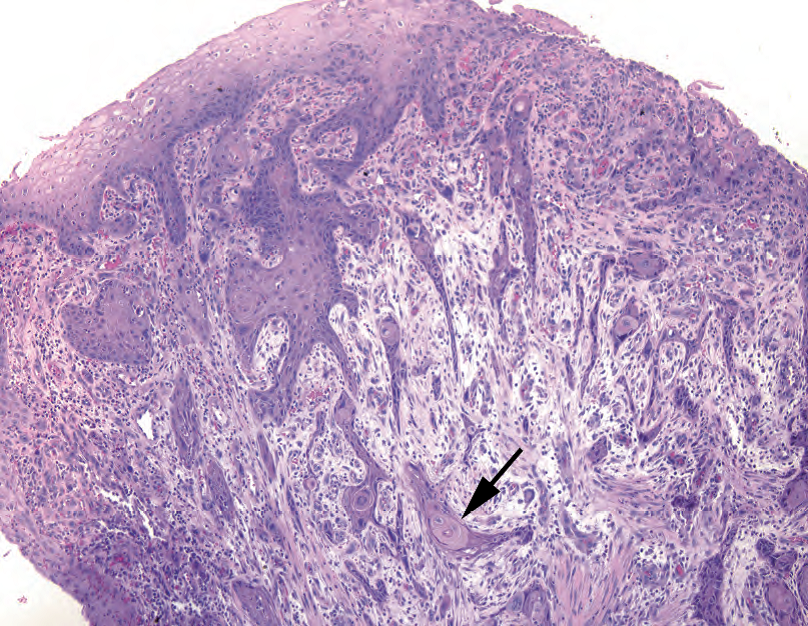
Figure 4.4. Invasive squamous cell carcinoma. Irregular nests and spicules of cells invade down into the stroma from the surface (top). Although single infiltrating cells are not visible at this magnification, the deep aberrant keratinization (arrow), in which a deep nest of cells takes on the color and texture of the normal surface keratin, is highly suspicious for invasion.
图4.4。浸润性鳞状细胞癌。细胞形成不规则的巢状和细针状结构,从表面(顶部)向下浸润至间质内。尽管在此放大倍数下无法看到单个浸润细胞,但深部异常角化(箭头所示),即深部细胞巢呈现正常表面角蛋白的颜色和质地,应高度怀疑浸润。
术语的定义(Definitions of Terms)
Hyperkeratosis: too much keratin, which sits on the epithelial surface in a thick pink layer, often accompanied by parakeratosis
角化过度:角蛋白过多,位于上皮表面的粉红色厚层中,常伴有角化不全
Inverted papilloma: endophytic growth of islands of benign squamous epithelium. The nests should be surrounded by stroma, and fibrovascular cores are not seen. Each nest is bordered by a smooth continuous basement membrane. It is essentially an inside-out papilloma.
内翻性乳头状瘤:良性鳞状上皮形成岛状结构,内生性生长。巢应当围绕着间质,未见纤维血管核心。每个巢外都有一层光滑连续的基底膜。本质上是由内而外(内外倒置)的乳头状瘤。
Orthokeratosis: “normal” keratin, found on the skin, with a basket weave pattern; anucleate
正常角化:皮肤上发现的“正常”角蛋白,呈网篮状编织模式;无核
Papilloma: exophytic growth of finger-like, arborizing projections with fibrovascular cores, lined by squamous epithelium (Figure 4.5)
乳头状瘤:指状树枝状突起的外生性生长,有纤维血管轴心,衬覆鳞状上皮(图4.5)
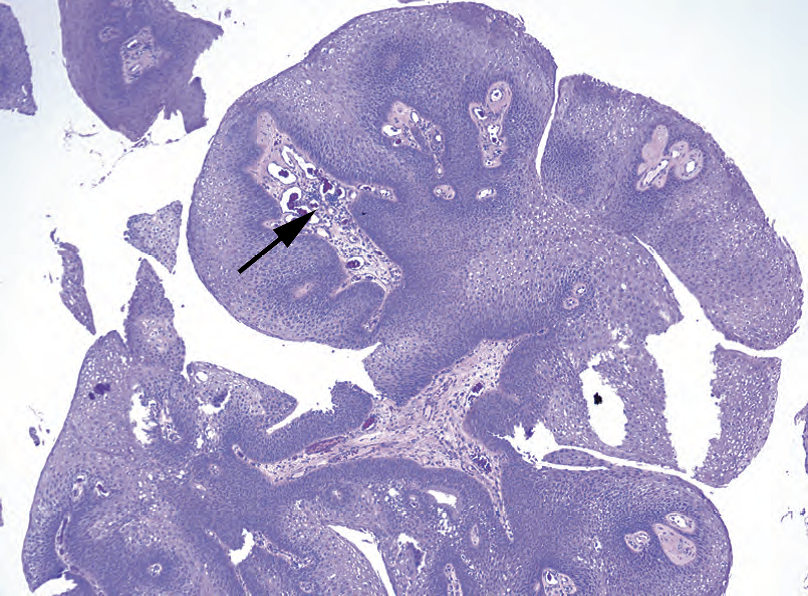
Figure 4.5. Papilloma. The squamous papilloma is defined by a squamous epithelium overlying branching fibrovascular cores (arrow).
图4.5。乳头状瘤。鳞状乳头状瘤定义为覆盖在分枝状纤维血管轴心(箭头)上的鳞状上皮。
Parakeratosis: the retention of small pyknotic nuclei in surface keratin
角化不全:表面角化物中保留小的固缩核
Pseudoepitheliomatous hyperplasia: a benign reactive condition that simulates invasive squamous cell carcinoma. It has a very characteristic look, as though someone dragged the epithelium down into the stroma with a toothpick, like marbling a cake (Figure 4.6). The individual nuclei should look reactive, not dysplastic. There should not be deep keratinization.
假上皮瘤样增生:一种良性反应性疾病,貌似浸润性鳞状细胞癌。它有一种非常独特的外观,就像有人用牙签把上皮拖到间质中,就像在蛋糕上刻划大理石花纹一样(图4.6)。单个细胞核应呈反应性,而不是异型增生。不应有深部角化。
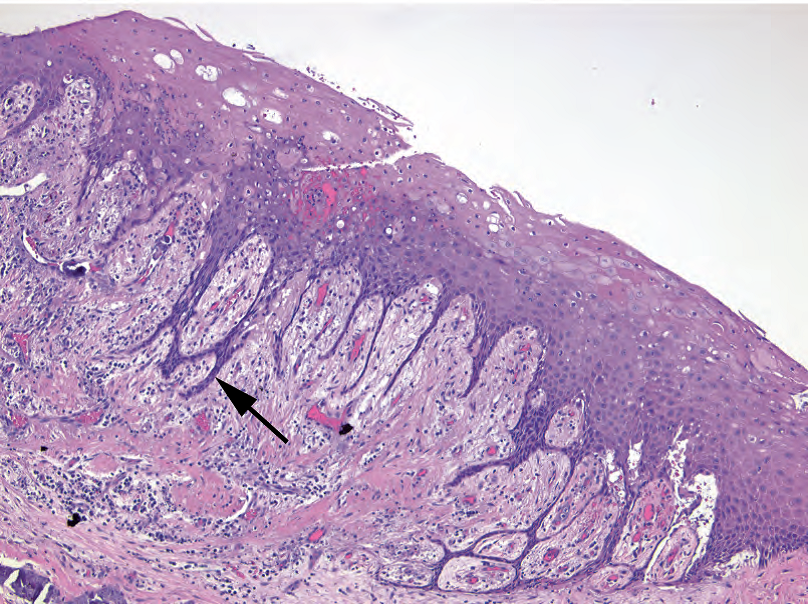
Figure 4.6. Pseudoepitheliomatous hyperplasia. In this reactive condition, thin strands of epithelium (arrow) are pulled down into the underlying dermis or lamina propria. However, the strands should not expand out into nests or show deep keratinization (compare to Figure 4.4).
图4.6。假上皮瘤样增生。在这种反应性疾病中,细长的上皮条(箭头所示)被拉下进入下面的真皮或固有层。然而,上皮条不应扩大成巢,也不显示深部角化(与图4.4相比)。
Verrucous: an exophytic growth pattern with prominent hyperkeratosis (Figure 4.7) and an appearance described as “church spire” (pointy projections) or “cauliflower” (rounded projections)
疣状:一种外生性生长模式,伴有明显的角化过度(图4.7),这种外观常被描述为“教堂尖顶”(尖形突出物)或“花菜”(圆形突出物)
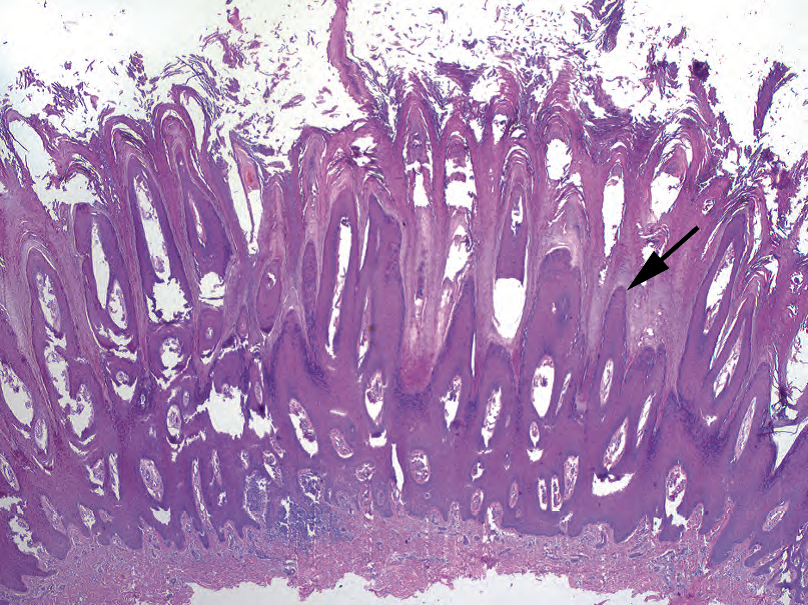
Figure 4.7. Verrucous pattern in a wart. Verruca vulgaris is characterized by prominent exophytic spires of the epidermis (arrow), with overlying hyperkeratosis and parakeratosis.
图4.7。疣的疣状模式。寻常疣的特征是表皮形成显著的外生性尖顶(箭头所示),伴有上方的角化过度和角化不全。
Cervix(子宫颈)
The cervix (discussed in detail in Chapter 16) is sort of the prototypical mucosal squamous epithelium. It can be closely studied, and the changes of dysplasia are well documented and well-understood. Dysplastic changes in the cervix are nearly all HPV-related, whereas reactive changes and squamous metaplasia are so common that they are considered normal. Dysplastic changes are grouped into low- and high-grade, with high-grade encompassing cervical intraepithelial neoplasia (CIN) grades 2 and 3. The low-grade squamous intraepithelial lesions (LSILs) show predominantly viral-type changes in the superficial epithelium and can regress. The high-grade lesions (HSILs) show significant dysplasia rising up from the basal layer and overtaking part or all of the epithelium. They are less likely to regress and are treated aggressively.
宫颈(在第16章详细讨论)是一种典型的粘膜鳞状上皮。它已被仔细研究,异型增生改变有大量描述和深入理解。宫颈的异型增生改变几乎都与HPV有关,而反应性改变和鳞状化生因为太常见而认为正常。异型增生病变分为低级别和高级别,高级别包括宫颈上皮内肿瘤(CIN)2级和3级。低度鳞状上皮内病变(LSIL)主要表现为浅层上皮的病毒型改变,并可消退。高度鳞状上皮内病变(HSIL)表现为明显的异型增生,从基底层向上生长,并超过部分或全部上皮。它们不太可能消退,应积极治疗。
(译注:neoplasia传统翻译为“肿瘤”是一种误解,想当然地认为含有肿瘤动态变化的意思。其实本义就是“肿瘤”,即新生物)
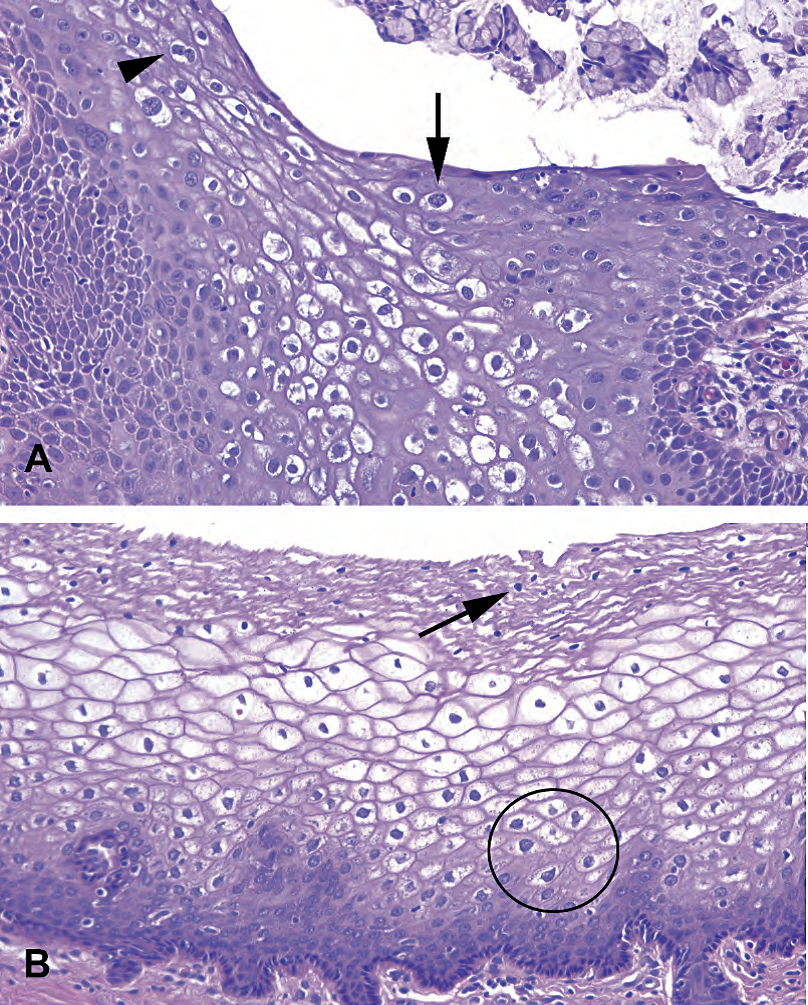
Figure 4.8. Viral or koilocytic atypia versus glycogen. (A) In this cervical lesion (low-grade squamous intraepithelial lesion [LSIL]), koilocytes are visible as large cells with prominent, crinkled, dark nuclei and perinuclear halos (arrow). Nuclei that get larger as you approach the surface are an indicator of dysplasia. Binucleate cells are suggestive of LSIL (arrowhead). (B) Normal glycogenated cervical epithelium can appear to have prominent nuclear halos, but the nuclei at the surface should be tiny and pyknotic (arrow). Larger cells may be seen near the basal layer (circle).
图4.8。病毒性细胞改变或非典型挖空细胞对比糖原。(A) 这个宫颈病变为低度鳞状上皮内病变(LSIL),挖空细胞表现为大细胞,细胞核明显、有皱褶、深染,并有核周空晕(箭头)。接近表面的核变大是异型增生的指标。双核细胞提示LSIL(箭头)。(B) 正常的糖原化宫颈上皮可能有明显的核周空晕,但其表层的细胞核应该很小且固缩(箭头所示)。基底层(圆圈)附近可见较大的细胞。
低度鳞状上皮内病变(CIN 1级)(Low-Grade Squamous Intraepithelial Lesions (Cervical Intraepithelial Neoplasia Type1))
Koilocytic (viral) changes, characterized by ballooned, cleared-out cells with enlarged, raisinoid nuclei, are present. Beware glycogenated normal cells, which are also ballooned but have small nuclei (Figure 4.8).
挖空细胞(病毒)改变,其特征为气球状、透明细胞和增大的葡萄干样核。小心糖原化正常细胞,它们也呈气球状,但核小(图4.8)。
The basal layer is disorganized, with mitoses in the lower one third of the epithelium.
基底层杂乱无序,核分裂象局限于上皮的下三分之一。
Condylomas have the same changes but a verrucous architecture.
尖锐湿疣也有同样的细胞学改变,但有疣状结构。
高度鳞状上皮内病变(CIN 2和CIN 3)(High-Grade Squamous Intraepithelial Lesions (Cervical Intraepithelial Neoplasia Types 2 and 3))
Undifferentiated, immature cells occupy > 50% of the epithelium (Figure 4.9).
未分化、未成熟细胞占据上皮的50%以上(图4.9)。
Mitoses occur above the lower one third of the epithelium.
核分裂发生在上皮的下三分之一的上方。
Overlying koilocytes or adjacent LSIL may be present.
可能存表层空泡细胞或相邻的LSIL。
Cells can be deceptively bland looking without prominent mitoses, but nuclei should still be enlarged with high N/C ratios.
细胞可能貌似温良,没有明显的核分裂,但核仍应增大、高N/C比。
Beware immature squamous metaplasia, which can look like HSIL at low power.
小心未成熟鳞状化生,在低倍镜下看似HSIL。
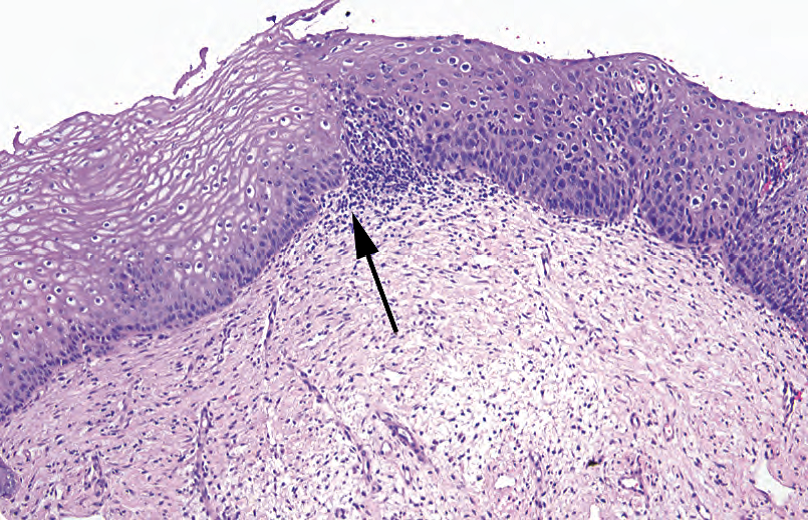
Figure 4.9. High-grade squamous intraepithelial lesion. An abrupt transition (arrow) is visible between normal (left) and dysplastic (right) epithelium. The epithelium at right shows a persistence of immature cells (large nuclei and high N/C ratios) up to the surface. Compare this to the clear distinction between basal cells and maturing cells seen at left.
图4.9。高度鳞状上皮内病变。在正常(左)和异型增生(右)上皮之间有一种突然转变(箭头)。右侧的上皮显示未成熟细胞(大核、高N/C比)一直持续到表面。将此与左侧所示的基底细胞和成熟细胞之间的明显区别进行比较。
Urothelium(尿路上皮)
The urothelium (discussed in detail in Chapter 12) when benign is five to seven cells thick, with an umbrella cell layer. Reactive changes look similar to those in other organs, and squamous metaplasia can also occur.
尿路上皮(在第12章详细讨论),良性有5-7层细胞厚度,表面有伞细胞层。反应性改变与其他器官相似,鳞状化生也可能发生。
Carcinoma arising in the urothelium can follow two pathways: flat and papillary. Flat lesions are those that progress from dysplasia to CIS to invasive carcinoma, without making an exophytic lesion; these are similar to epithelia in other sites. Papillary lesions, however, are graded as benign (papilloma), borderline (papillary urothelial neoplasm of low malignant potential), or cancer (low- and high-grade papillary urothelial carcinoma) based on histologic features.
尿路上皮发生的癌有两条途径:平坦和乳头状。平坦病变是从异型增生到原位癌再到浸润性癌,而没有外生性病变;这些形态学变化类似于其他部位上皮的癌变过程。而乳头状病变,根据组织学特征分为良性(乳头状瘤)、交界性(低度恶性潜能乳头状尿路上皮肿瘤)或癌(低级别和高级别乳头状尿路上皮癌)。
Although most papillary cancers are in situ, by convention papillary cancers are called invasive or noninvasive. Carcinoma in situ refers only to flat lesions. The term dysplasia is also not applied to papillary lesions, as there is a fairly low threshold for calling low-grade carcinoma.
尽管大多数乳头状癌是原位癌,但根据惯例乳头状癌被称为浸润性或非浸润性癌。原位癌仅指平坦病变。异型增生一词也不适用于乳头状病变,因为称为低级别癌的门槛相当低。
Do not be fooled by the von Brunn’s nests. These are invaginated folds of normal urothelium, which can simulate invasion.
不要被von Brunn巢所愚弄。这些是正常尿路上皮的内陷,可能貌似浸润。
Features of urothelial carcinoma include the following:
尿路上皮癌的特征包括:
Increased number of cell layers (mainly in papillary lesions)
细胞层数量增加(主要在乳头状病变中)
Loss of polarity (loss of parallel arrays of nuclei)
失去极性(核不再平行排列)
Increased mitoses, above the basal layer
基底层以上核分裂增多
Enlarged, irregular, or hyperchromatic nuclei
核增大、不规则或深染
Discohesive cells or partially denuded epithelium
失黏附细胞或部分脱落的上皮
Oropharynx, Larynx, Tongue(口咽、喉、舌)
Squamous papillomas are relatively common in the larynx. Features of benign papillomas include hyperkeratosis (para or ortho), basal layer hyperplasia, abnormal mitoses, and koilocytic changes (HPV change). They should not have significant atypia, high-grade dysplasia, or warty architecture (church-spire keratosis).
鳞状上皮乳头状瘤在喉部比较常见。良性乳头状瘤的特征包括角化过度(角化不全或正常角化)、基底层增生、异常核分裂和挖空细胞改变(HPV改变)。它们不应该有显著非典型、高度异型增生或疣状结构(教堂尖顶状角化病)。
The mouth and larynx are lined by a nonkeratinized squamous epithelium, like the cervix. Unlike the cervix, however, the oral mucosa tends to keratinize in dysplasia. This leads to a different pattern of dysplasia called severe keratinizing dysplasia. In severe keratinizing dysplasia, the dysplasia does not have to be full thickness to behave like CIS, so it is a more insidious lesion. The criteria for grading dysplasia are much more subjective than in the cervix.
口腔和喉部被覆一层非角化鳞状上皮,就像宫颈。然而,与宫颈不同,口腔粘膜在异型增生时往往角化。这导致一种不同模式的异型增生,称为重度角化性异型增生。在重度角化性异型增生中,异型增生不一定是全层厚度的,而生物学行为像原位癌,因此它是一种更隐蔽的病变。异型增生分级的标准比宫颈更加主观。
Features of squamous dysplasia in the mouth include the following:
口腔鳞状异型增生的特征包括:
Loss of polarity of basal layer and maturation arrest (basal-type cells above the basal layer)
基底层失去极性和成熟停滞(基底层以上出现基底型细胞)
Dyskeratosis (abnormal keratinization), hyperkeratosis, and acanthosis
角化不良(异常角化)、角化过度和棘皮病
Increased mitoses and/or mitoses above the basal layer
核分裂增多和/或基底层以上核分裂
Cellular and nuclear pleomorphism (unlike at many other sites, dysplastic nuclei tend to show prominent nucleoli and nuclear membranes, almost like an invasive carcinoma; Figure 4.10)
细胞和核多形性(与许多其他部位不同,异型增生核往往显示显著的核仁和核膜,很像浸润性癌;图4.10)
Variable N/C ratios (in keratinizing dysplasia, there may be abundant pink cytoplasm)
N/C比可变(在角化性异型增生中,可能有丰富的粉红色细胞质)
Not necessarily full-thickness involvement, even in severe dysplasia
不一定全层受累,即使重度异型增生也是如此
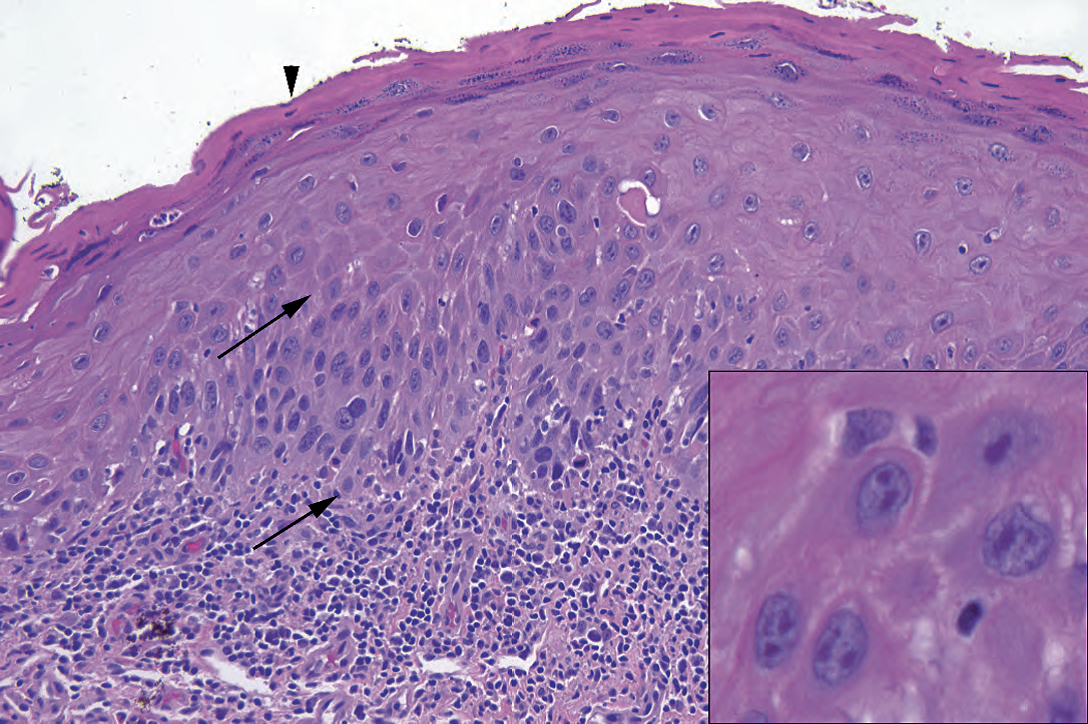
Figure 4.10. Squamous dysplasia in the mouth. In the area between the arrows, dysplastic cells with high N/C ratios and hyperchromatic, irregular nuclei can be seen occupying the lower half of the epithelium. The surface shows parakeratosis (arrowhead), which clinically will appear as a white plaque. Inset: Unlike in cervical dysplasia, prominent nucleoli are often seen in keratinizing dysplasia of the oral cavity. Notice the irregularly shaped nuclear membranes.
图4.10。口腔鳞状细胞异型增生。在箭头之间的区域,可以看到异型增生细胞伴高N/C比和深染,不规则核占据上皮的下半部分。表面显示角化不全(箭头),临床上表现为白斑。插图:与宫颈异型增生不同,口腔角化性异型增生常见显著的核仁。注意形状不规则的核膜。
Nasopharynx(鼻咽)
Schneiderian (sinonasal) papillomas are characterized by the following:
施奈德(鼻窦)乳头状瘤的特征如下:
They are lined with a nonkeratinizing squamous or intermediate epithelium, 5–30 cells thick, and may have a ciliated or mucous lining (Figure 4.11). Neutrophils are common.
它们被覆非角化鳞状上皮或中间上皮,5-30层细胞厚度,表面可能被覆纤毛细胞或粘液细胞(图4.11)。中性粒细胞很常见。
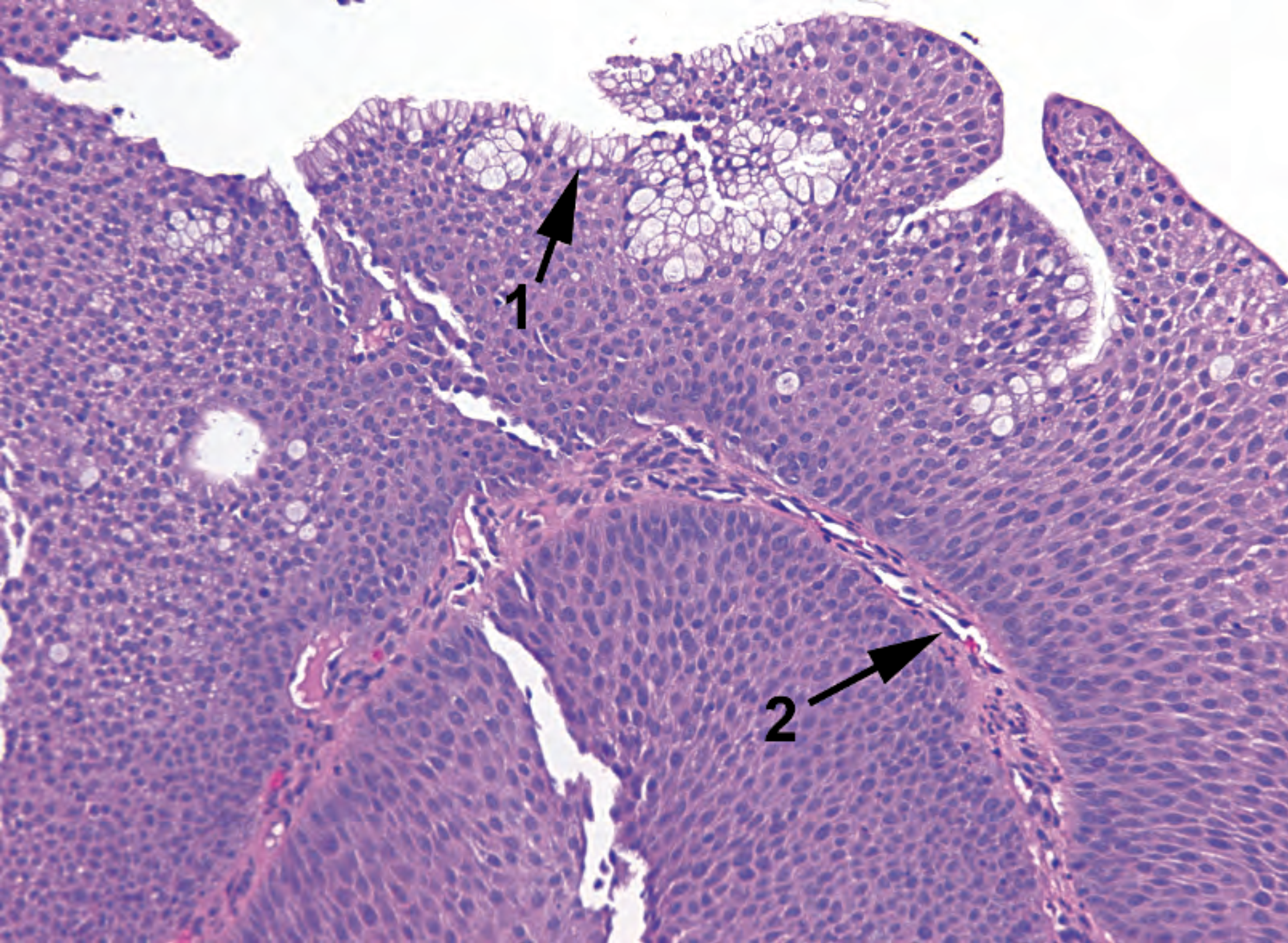
Figure 4.11. Schneiderian papilloma. The typical features are a squamous or respiratory epithelium with goblet cells (1) and neutrophils (not seen at this power). As in any papilloma, there are fibrovascular cores (2).
图4.11。施奈德乳头状瘤。典型特征是鳞状上皮或呼吸上皮,有杯状细胞(1)和中性粒细胞(这种放大倍数看不到)。与任何乳头状瘤一样,也有纤维血管轴心(2)。
They may be fungiform (exophytic, septal) or inverted (inward growing).
它们可能是蕈状(外生,有间隔)或内翻(向内生长)。
They should have only mild atypia, orderly cells, and few mitoses.
它们应该只有轻微非典型性,细胞排列有序,只有极少核分裂。
The differential diagnosis for an inverted papilloma includes an invasive squamous carcinoma. Atypia and pleomorphism, increased mitotic activity, and cells invading as nests and cords should be present.
内翻性乳头状瘤的鉴别诊断包括浸润性鳞癌。鳞癌应出现非典型性和多形性,核分裂活性增加,细胞呈巢状和条索状浸润。
Trachea and Bronchi(气管与支气管)
Respiratory epithelium undergoes squamous metaplasia when irritated. Dysplastic lesions may then arise from the squamous epithelium.
受刺激时,呼吸上皮发生鳞状化生。然后鳞状上皮可能出现异型增生病变。
Esophagus(食管)
In the esophagus (which is discussed in detail in Chapter 6), the squamous mucosa is not usually the bad actor; dysplasia is more often seen in the setting of Barrett’s esophagus.
在食道(第6章详细讨论),鳞状上皮粘膜通常不是坏蛋主角;异型增生更常见于Barrett食管。
Mild reactive changes are very common, and correspond to reflux changes. More intense reactive changes can be seen in infection.
轻微的反应性改变很常见,对应于反流改变。在感染中可以看到更强烈的反应性改变。
Squamous dysplasia is not often seen on biopsy, as it is asymptomatic. Squamous carcinoma looks similar to that found in other sites.
鳞状细胞异型增生不常见于活检,因为无症状。鳞状细胞癌与其他部位相似。
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。
本站欢迎原创文章投稿,来稿一经采用稿酬从优,投稿邮箱tougao@ipathology.com.cn
相关阅读
 数据加载中
数据加载中
我要评论

热点导读
-

淋巴瘤诊断中CD30检测那些事(五)
强子 华夏病理2022-06-02 -

【以例学病】肺结节状淋巴组织增生
华夏病理 华夏病理2022-05-31 -

这不是演习-一例穿刺活检的艰难诊断路
强子 华夏病理2022-05-26 -

黏液性血性胸水一例技术处理及诊断经验分享
华夏病理 华夏病理2022-05-25 -

中老年女性,怎么突发喘气困难?低度恶性纤维/肌纤维母细胞性肉瘤一例
华夏病理 华夏病理2022-05-07






共0条评论