外科病理学实践:诊断过程的初学者指南 | 第3章 感染和炎症
第3章 感染和炎症
Let us review the types of inflammatory responses you may see. It seems very basic, but learning to differentiate inflammatory changes from dysplastic ones is a fundamental goal in pathology training.
先复习一下,你可能会看到的炎症反应类型。这似乎非常基础,但学会区分炎症改变和异型增生改变是病理学培训的基本目标。
3.1 急性(Acute)
Acute changes are the result of recent tissue damage, either from trauma, ischemia, toxins, or infection. Features include the following:
急性炎症改变是近期组织损伤的结果,病因包括创伤、缺血、毒素和感染,等。其特点包括:
血管充血(Vascular congestion)
水肿(Edema)
纤维素性渗出物(Fibrinous exudate)
组织损伤和/或坏死(Tissue damage and/or necrosis)
中性粒细胞(“化脓性”,多形核白细胞,简写polys)(Neutrophils (“purulence”, polymorphonuclear leukocytes, polys))
Acute inflammation can be followed by resolution (healing), fibrosis or scar, abscess formation (Figure 3.1), or a chronic inflammatory stage. Evidence of recent damage and reparative changes includes granulation tissue, hemosiderin, lipid-laden macrophages, and fibroblast proliferation.
急性炎症后可以消退(愈合)、纤维化或形成瘢痕、脓肿(图3.1),或转变成慢性炎症。近期损伤和修复性改变的证据包括肉芽组织、含铁血黄素、富含脂质的巨噬细胞和成纤维细胞增殖(译者注:注意比较hyperplasia,增生)。
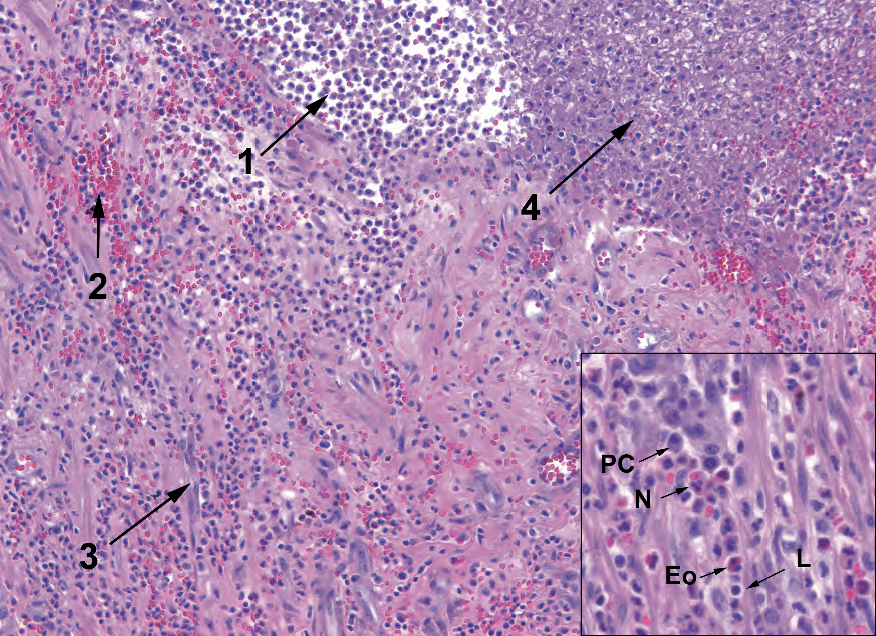
Figure 3.1. Acute inflammation and abscess formation. This example of the acute inflammatory response shows collections of neutrophils (abscess formation, 1), extravasated blood (2), prominent capillaries (3), and fibrin accumulation (4). Inset: the mixed inflammatory infiltrate includes plasma cells (PC), neutrophils (N), eosinophils (Eo), and lymphocytes (L).
图3.1.急性炎症和脓肿形成。这例急性炎症反应显示中性粒细胞聚集(脓肿形成,1)、渗出的血液(2)、显著的毛细血管(3)和纤维素积聚(4)。插图:混合性炎症细胞浸润,包括浆细胞(PC)、中性粒细胞(N)、嗜酸性粒细胞(Eo)和淋巴细胞(L)。
Granulation tissue has a characteristic look of a watery or myxoid background with sparse fibroblasts floating in it and a proliferation of inflammatory cells (all types) and capillaries (Figure 3.2). The endothelial cells of the capillaries can become quite prominent.
肉芽组织具有特征性表现:水样或粘液样背景,稀疏的成纤维细胞漂浮在其中,炎症细胞(所有类型)和毛细血管增殖(图3.2)。毛细血管的内皮细胞可以变得非常显著。
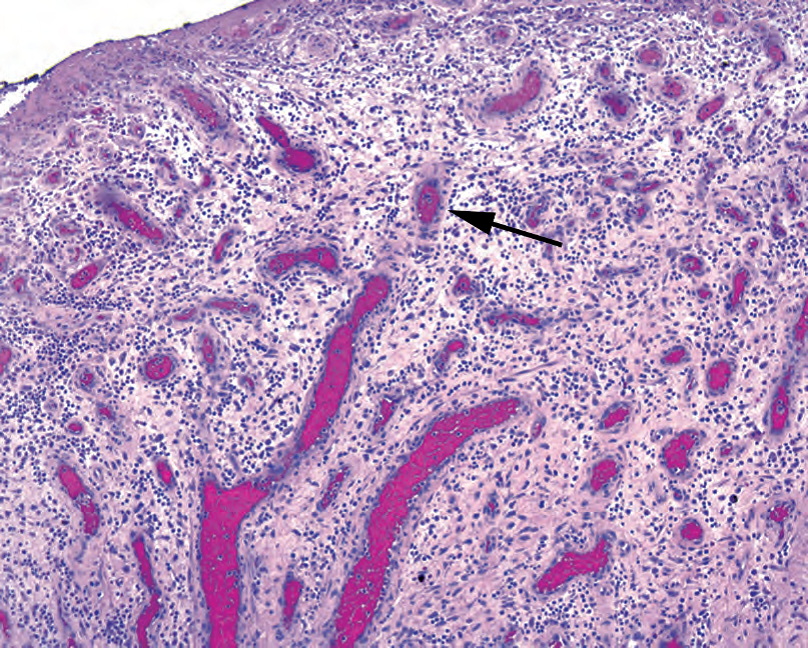
Figure 3.2. Granulation tissue is characterized by a loose myxoid background with fibroblasts and inflammatory cells and by prominent capillaries with plump endothelial cells and thick walls. The stroma appears condensed and thickened around the capillaries, giving them a pink halo (arrow).
图3.2.肉芽组织的特征是疏松的黏液样背景,有成纤维细胞和炎症细胞,显著的毛细血管伴有丰满的内皮细胞和厚的血管壁。间质在毛细血管周围显得浓缩和增厚,形成粉红色光晕(箭头)。
Biopsy site changes, a term often used to indicate evidence of a recent procedure, include fibroblast proliferation (early scar), foreign body–type giant cells, suture material, foamy macrophages, fat necrosis, and inflammation. They have a more solid look to them than granulation tissue (Figure 3.3).
活检部位改变,这个术语常用于描述近期手术证据,包括成纤维细胞增殖(早期瘢痕)、异物型巨细胞、缝合材料、泡沫状巨噬细胞、脂肪坏死和炎症。与肉芽组织相比,它们看起来更加坚实(译者注:常用词solid,坚实的,实性,实质性,实体性,大体描述一种质地较硬但不到坚硬的程度,镜下描述细胞较丰富,结构较紧凑)(图3.3)。
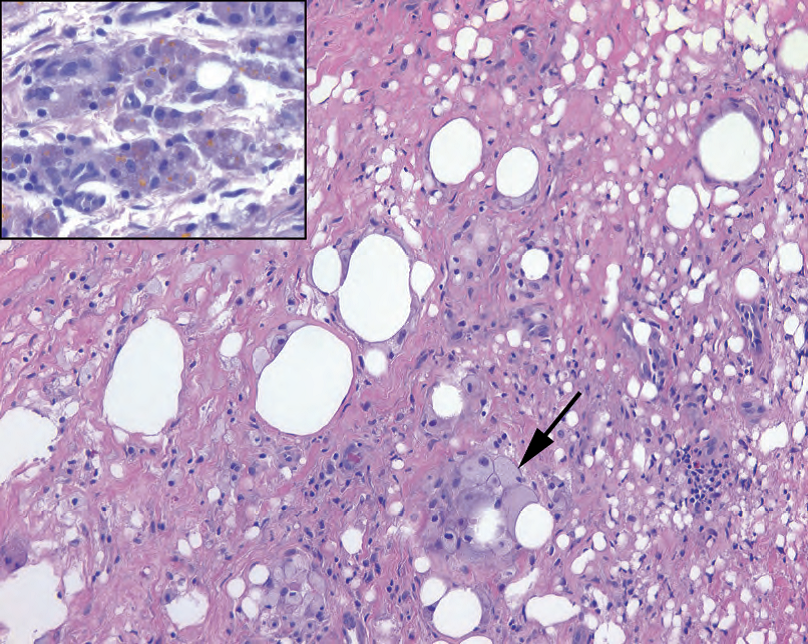
Figure 3.3. Biopsy site changes. In this subcutaneous specimen, collagen has replaced most of the fat cells, and foamy histiocytes can be seen ingesting some residual fat (arrow). Inset: Hemosiderin in macrophages (golden yellow to brown granules) can be seen in sites of prior trauma or bleeding.
图3.3.活检部位改变。在这个皮下标本中,胶原蛋白已经取代了大部分脂肪细胞,可以看到泡沫组织细胞摄取了一些残留的脂肪(箭头)。插图:在先前的创伤或出血部位可以看到巨噬细胞中的含铁血黄素(金黄色至棕色颗粒)。
Scar tissue implies that a dense thick collagen has replaced the normal structures. In the skin, a dermal scar is evidenced by a homogeneous pink layer of collagen and absence of adnexal structures (Figure 3.4).
瘢痕组织是指一种致密的厚胶原已经取代了正常的结构。在皮肤中,瘢痕表现为一层均匀的粉红色胶原,没有附属器结构(图3.4)。
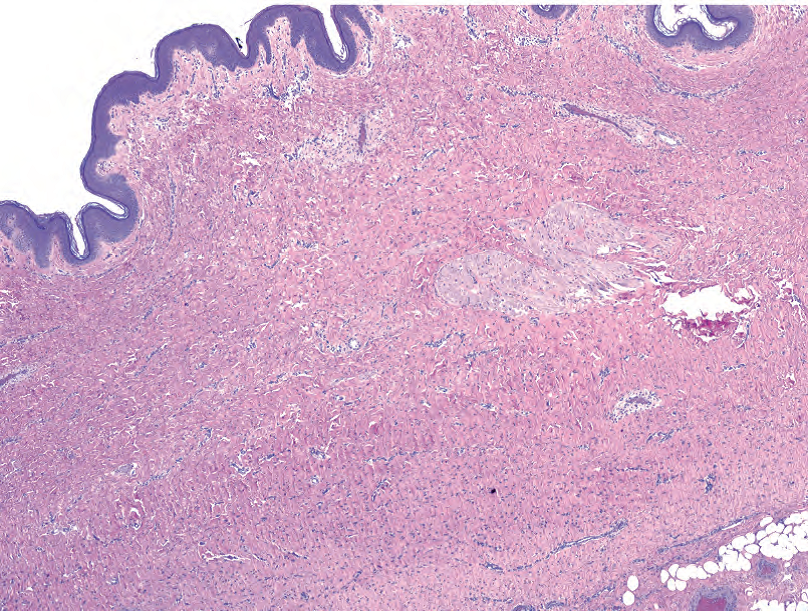
Figure 3.4. Dermal scar. Dense pink collagen has replaced the adnexal structures and displaced the subcutaneous fat in this biopsy site.
图3.4.皮肤瘢痕。致密的粉红色胶原已经取代了附属器结构,并取代了活检部位的皮下脂肪。
3.2 慢性(Chronic)
Chronic changes are the result of repetitive or sustained tissue damage due to trauma, ischemia, toxins, infection, or autoimmune processes. Features include the following:
慢性炎症改变是由于创伤、缺血、毒素、感染或自身免疫疾病引起的重复性或持续性组织损伤的结果。其特点包括:
血管增多和/或纤维化(试图愈合)(Increased vascularity and/or fibrosis (attempts to heal))
组织破坏(Tissue destruction)
淋巴细胞、巨噬细胞、浆细胞、嗜酸性粒细胞(Lymphocytes, macrophages, plasma cells, eosinophils)
What is a macrophage? The precursor is a circulating monocyte, part of the myeloid lineage of blood cells (myeloid generally refers to cells in the granulocyte and monocyte groups, although it can also mean all cells that mature in the bone marrow, i.e., the opposite of lymphoid). The monocyte leaves the circulation and becomes a tissue macrophage. It can differentiate into organ-specific resident macrophages, such as microglia, Kupffer cells, and alveolar macrophages. It can also go to an area of inflammation and become activated, participating in the immune response. Activated macrophages are also called histiocytes and may be “epithelioid,” as in a granuloma, or “foamy,” as in lipid-laden or xanthomatous. Finally, macrophages can acquire multiple nuclei to become a Langerhans giant cell (ring of nuclei) or a foreign body–type giant cell (scattered nuclei).
什么是巨噬细胞?其前体是血液循环中的单核细胞,是血细胞中髓系细胞的一部分(髓系通常指粒细胞和单核细胞群中的细胞,尽管它也可以指在骨髓中成熟的所有细胞,即,相对于淋巴细胞系)。单核细胞离开循环,成为组织巨噬细胞。它可以分化为器官特异性常驻巨噬细胞,如小胶质细胞、库弗细胞和肺泡巨噬细胞。它也可以进入炎症区域并被激活,参与免疫反应。活化的巨噬细胞也称为组织细胞,可能呈“上皮样”,如肉芽肿;也可能呈“泡沫状”,如富含脂质的组织细胞或黄色瘤中的组织细胞。最后,巨噬细胞可以获形成多核,形成朗格汉斯巨细胞(核排列成环形)或异物型巨细胞(核散在分布)。
(译者注:注意原文笔误,多核组织细胞或多核巨细胞应为Langhans(朗罕)巨细胞,而Langerhans(郎格汉斯)细胞是一种树突状细胞,功能上属于抗原提呈细胞)
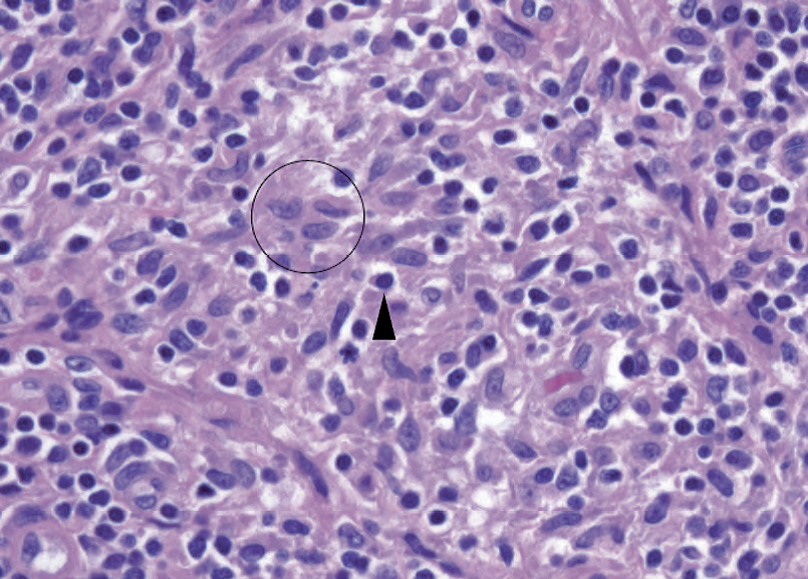
Figure 3.5. Histiocytes appear as pale folded nuclei within an area of inflammation; the cell borders are indistinct, but the nuclei are surrounded by light pink cytoplasm (circle). Compare the pale chromatin to that of the neighboring lymphocyte (arrowhead).
图3.5.组织细胞在炎症区域内表现为淡染的折叠细胞核;细胞边界模糊,但细胞核被淡粉色细胞质包围(圆圈)。将淡染的染色质与相邻淋巴细胞(箭头)的染色质进行比较。
Histologically, histiocytes have a bland and fade-into-the-background look to match their name (literally, “tissue cell”). They have pale-pink granular cytoplasm, sometimes with chunky phagocytosed bits of material, and indistinct cell borders (Figure 3.5). The nuclei are light with crisp outlines, oval in shape, and often grooved. In tissue, a collection of histiocytes appears as an ill-defined pink area that is easy to miss. The nuclei often stream in a circular pattern like fish swimming in a barrel. Foamy macrophages are stuffed with lipid debris or organisms, and can have an almost signet-ring appearance.
组织学上,组织细胞的形态学温和,淡入背景,很匹配其名称(字面意思就是“组织细胞”)。它们有淡粉色颗粒性细胞质,有时有大块被吞噬的物质,细胞边界模糊(图3.5)。细胞核较淡,轮廓清晰,呈椭圆形,常有凹槽。在组织中,组织细胞的聚集表现为一个界限不清的粉红色区域,很容易被忽略。细胞核通常呈环形流动,就像鱼在桶中游泳一样。泡沫状巨噬细胞内充满脂质碎片或微生物,可能很像印戒状外观。
What are eosinophils? Eosinophils have a bilobed nucleus and big red granules. They are usually an indication of an immune/IgE response, such as to drug allergy or parasites.
什么是嗜酸性粒细胞?嗜酸性粒细胞有双叶核和大的红色颗粒。它们通常提示免疫反应/IgE反应,例如药物过敏或寄生虫。
We usually refer to the presence of lymphocytes as chronic inflammation. Lymphocytes plus neutrophils equals acute and chronic inflammation. In the gastrointestinal tract, instead of acute we use active, such as active chronic gastritis or active chronic inflammatory bowel disease. Inactive in the gastrointestinal tract means increased lymphocytes but no polys.
我们通常将存在淋巴细胞的炎症称为慢性炎症。淋巴细胞加中性粒细胞等于急性和慢性炎症。在胃肠道中,我们不称为急性,而是称为活动性,如活动性慢性胃炎或活动性慢性炎症性肠病。胃肠道内无活动性炎症是指淋巴细胞增多,但中性粒细胞不增多。
3.3 肉芽肿性(Granulomatous)
A granulomatous appearance indicates a specific type of chronic inflammation with a small differential; it can be a result of mycobacteria (plus a few other bacteria), fungal infection, autoimmune disease, some toxins or irritants, and sarcoid. Granulomas are divided into caseating (usually infectious) and noncaseating.
肉芽肿性形态提示一种特殊类型的慢性炎症,但差别不大;它可能是由分枝杆菌(加上其他几种细菌)、真菌感染、自身免疫性疾病、某些毒素或刺激物以及结节病引起的。肉芽肿分为干酪样(通常为感染性)和非干酪样。
The histologic appearance of a granuloma is a microscopic aggregate of histiocytes, with surrounding lymphocytes and plasma cells. The appearance ranges from tiny collections of histiocytes (as in Crohn’s disease; Figure 3.6), to large well-circumscribed whorls of cells (sarcoid; Figure 3.7), to a layer of histiocytes surrounding a pool of caseous necrosis (tuberculosis, fungus; Figure 3.8). Giant cells are helpful but not essential. Old granulomas can become hyalinized and acellular (Figure 3.9).
肉芽肿的组织学表现为组织细胞的显微镜下聚集,周围有淋巴细胞和浆细胞。范围从微小的组织细胞聚集(如克罗恩病;图3.6),到边界清晰的旋涡状细胞聚集(结节病;图3.7),再到一层组织细胞围绕着干酪样坏死池(结核、真菌;图3.8)。巨细胞是有助于识别,但不是必需的。陈旧性肉芽肿可能变得透明和无细胞(图3.9)。
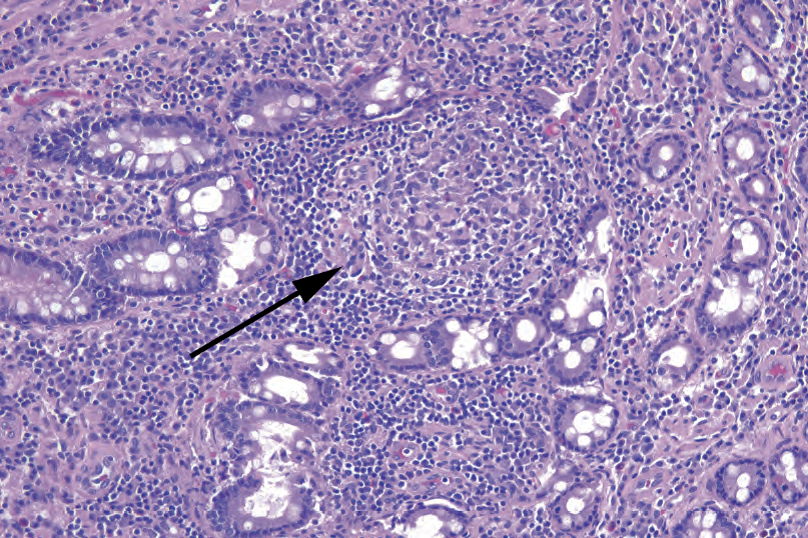
Figure 3.6. Granulomas in Crohn’s disease. These granulomas of the colon are subtle (arrow), and the pale histiocytes may be seen only on high power. A surrounding collar of lymphocytes is common.
图3.6.克罗恩病的肉芽肿。结肠的这些肉芽肿很轻微(箭头所示),只有在高倍镜下才能看到淡染的组织细胞。周围常见衣领状淋巴细胞围绕。
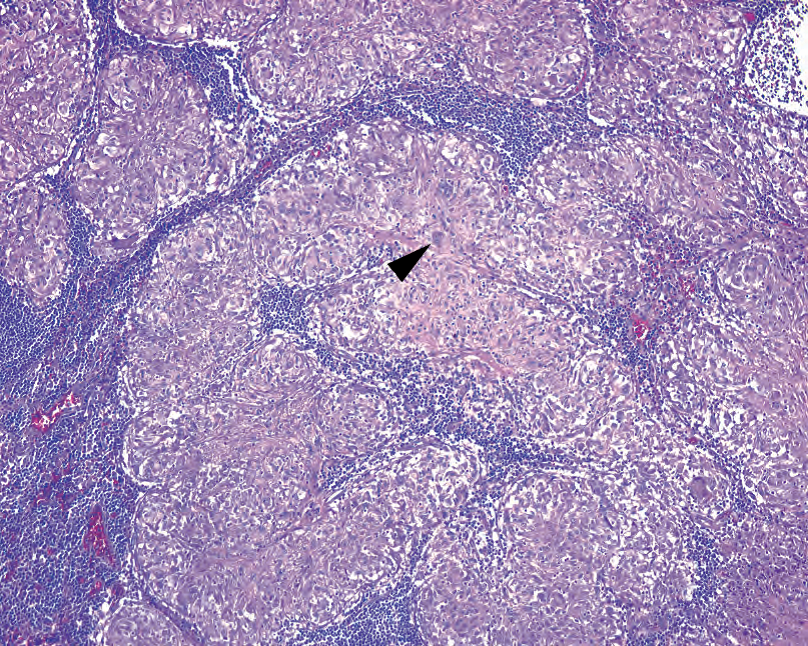
Figure 3.7. Granulomas in sarcoid. These granulomas are often more substantial and more easily recognized than those in Crohn’s disease. They appear as well-defined masses of pink histiocytes. Occasional multinucleated giant cells (arrowhead) are present.
图3.7.结节病的肉芽肿。与克罗恩病的肉芽肿相比,这些肉芽肿通常更明显,更容易识别。它们表现为边界清晰的粉红色组织细胞团块。偶尔出现多核巨细胞(箭头)。
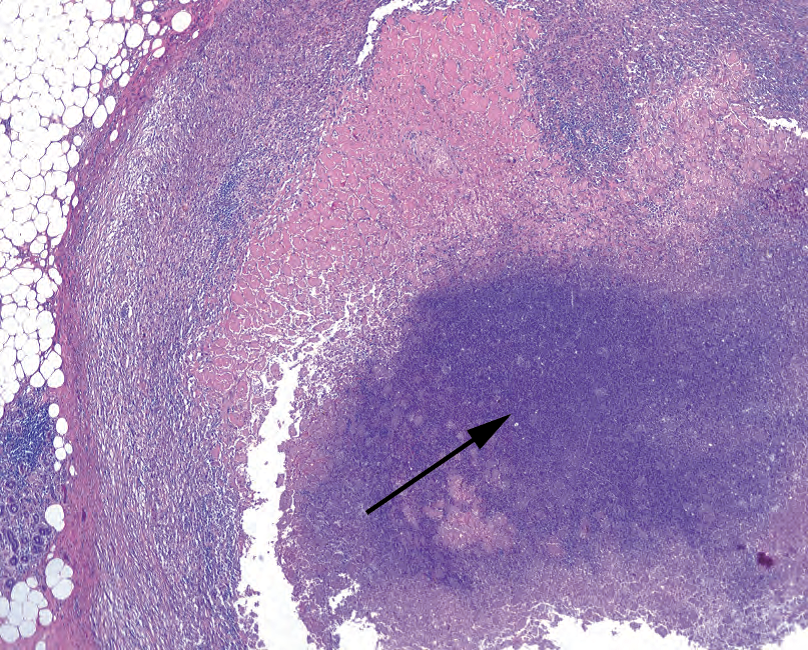
Figure 3.8. Caseating granulomas in tuberculosis. The histiocytes in these granulomas are visible only at the periphery, as the center is a mass of necrosis and cellular debris (arrow).
图3.8.结核中的干酪样肉芽肿。这些肉芽肿中的组织细胞仅在周围可见,因为中心是一团坏死和细胞碎片(箭头)。
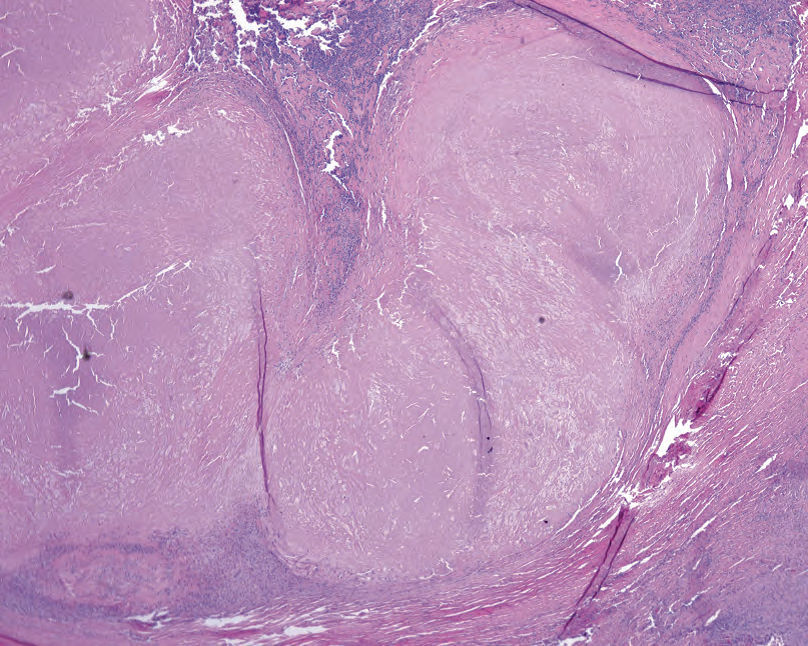
Figure 3.9. Hyalinized granuloma. The amorphous area of hyalinized collagen likely represents old, burned-out necrosis.
图3.9.玻璃样变的肉芽肿。透明变性的胶原形成无定形区域,可能代表陈旧性、燃烬的坏死。
3.4 特殊微生物及其染色(Specific Organisms and Their Stains)
3.4.1 真菌(Fungi)
Fungal organisms stain bright pink on periodic-acid Schiff (PAS) stain and black on Gomori’s methenamine silver (GMS) stain. For most of these organisms, it is important to identify not just the presence and morphology of the organism but whether it is invading viable tissue or colonizing necrotic debris. Size can be helpful in identifying the various yeasts (Figure 3.10).
真菌病原体在高碘酸希夫(PAS)染色上呈明亮的粉红色,在Gomori六胺银(GMS)染色上呈黑色。对于这些病原体中的大多数,重要的是不仅要识别病原体的存在和形态,还要确定它是入侵活组织还是定植在坏死碎片。大小有助于识别各种酵母(图3.10)。
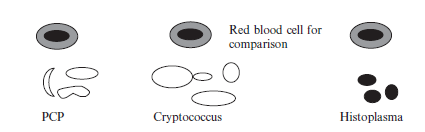
Figure 3.10. Relative size of yeasts.
图3.10.酵母的相对大小。
图中文字:
Red blood cell for comparison:红细胞用于比较大小
PCP:肺孢子菌肺炎,全称pneumocystis pneumonia(译注:此处应为Pneumocystis,肺孢子菌)
Cryptococcus:隐球菌
Histoplasma:组织胞浆菌
Candida are visible on HE as round-to-oval yeast forms and pseudohyphae (segmented and nonbranching). They are often found in the debris at the epithelial surface (Figure 3.11).
念珠菌在HE上可见,表现为圆形到椭圆形酵母形式和假菌丝(分段和非分枝)。它们通常出现在上皮表面的碎屑中(图3.11)。
Aspergillus are visible on HE as long, thin hyphae with 45° branching and septations. They may appear as a solid fungal ball or as single hyphae in the tissue (Figure 3.12). Treated Aspergillus may have different morphology.
曲霉茵在HE上可见,表现为细长的菌丝,具有45°分枝和分隔。它们在组织中可能表现为实心真菌球或单个菌丝(图3.12)。经处理的曲霉菌可能具有不同的形态。
Mucor and zygomycetes are irregular and wide nonseptate hyphae and have the appearance of gnarled tree branch outlines with wide branch points (Figure 3.13). On HE, they can be almost invisible, as they are essentially wide hollow spaces in the tissue. These are the bread molds and are typically seen only in very neutropenic patients or in sinusitis in a patient with ketoacidosis.
毛霉菌和接合菌表现为不规则的宽的非分隔菌丝,具有多节树枝轮廓和宽分枝点的外观(图3.13)。在HE上几乎看不到,因为它们本质上是组织中很宽的中空空隙。这些是面包霉菌,通常仅见于中性粒细胞减少症患者或酮症酸中毒患者的鼻窦炎。
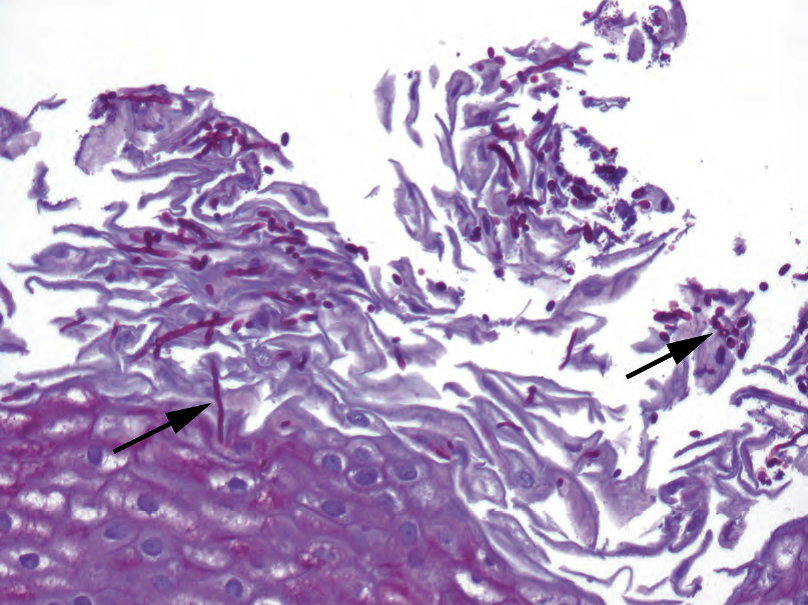
Figure 3.11. Candida. This example from the esophagus shows magenta pseudohyphae and yeasts (arrows, periodic-acid Schiff stain).
图3.11.念珠菌。病例取自食道,显示了品红色假菌丝和酵母(箭头,PAS染色)。
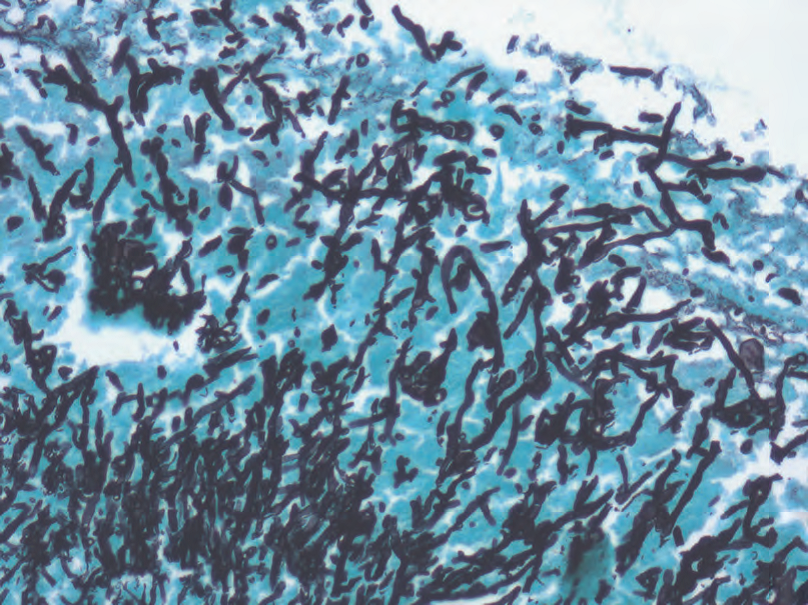
Figure 3.12. Aspergillus. A forest of branching hyphae are visible by Gomori’s methenamine silver stain.
图3.12.曲霉属。Gomori六胺银染色可以看到一片分枝的菌丝。
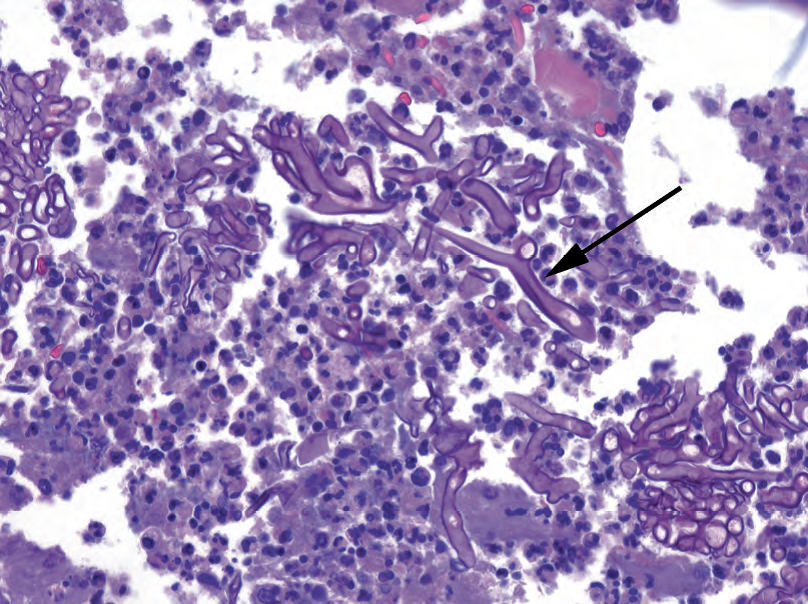
Figure 3.13. Mucor. A periodic-acid Schiff stain shows the thick, “hollow,” irregular outlines of Mucor (arrow).
图3.13.毛霉菌。PAS染色显示毛霉呈厚实、中空、不规则轮廓(箭头)。
Histoplasma are tiny intracellular yeast forms with narrow-based budding, often seen in macrophages. On HE and Giemsa stain, these are delicate 2-µm forms in macrophages. In the context of a hyalinized granuloma, however, a silver stain shows distinct yeasts that are nearly the size of red cells (about 5 µm; Figure 3.14).
组织胞浆菌是一种微小的细胞内酵母形式,具有基底狭小的出芽,常见于巨噬细胞内。在HE和Giemsa染色上,它们表现为巨噬细胞中精致的2µm酵母形式。然而,在玻璃样变肉芽肿的背景中,银染显示接近红细胞大小的确定无疑的酵母(约5µm;图3.14)。
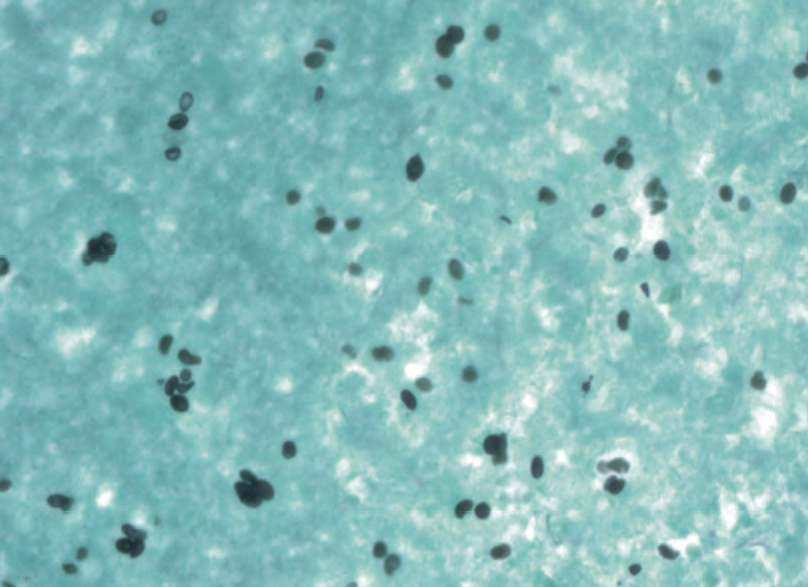
Figure 3.14. Histoplasmosis. Tiny yeasts are visible on Gomori’s methenamine silver stain (40× objective).
图3.14.组织胞浆菌病。在Gomori六胺银染色上可以看到微小的酵母(40x)。
Cryptococcus are usually encapsulated yeast forms with narrow-based budding; some may be in macrophages but are often free in the tissue; on GMS the sizes are variable, and some may collapse into squashed balls (Figure 3.15). This variability in size is actually a key indicator of Cryptococcus. Stains for the capsule of Cryptococcus can differentiate it from other yeasts, including mucicarmine and Fontana-Masson. However, be aware that Cryptococcus can occasionally lose the capsule.
隐球菌通常是有包膜的酵母形式,具有基底狭小的出芽;有些可能存在于巨噬细胞中,但通常是游离在组织中;在GMS上其大小可变,有些可能塌陷成受挤压的球状(图3.15)。这种大小的变化实际上是隐球菌的一个关键指标。隐球菌荚膜的染色可以区分其他酵母菌,包括黏液卡红染色和Fontana-Masson染色。然而,要注意隐球菌有时会失去荚膜。
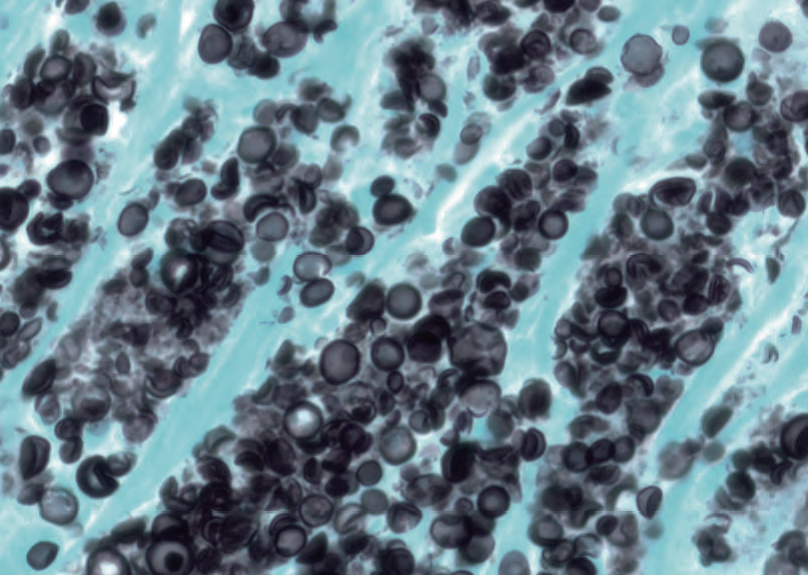
Figure 3.15. Cryptococcus. This photograph is taken at the same magnification as Figure 3.14. The organisms are significantly larger and show a range of sizes and shapes on Gomori’s methenamine silver stain.
图3.15.隐球菌。这张照片的放大倍数与图3.14相同。在Gomori六胺银染色上,这些病原体明显更大,并显示出各种大小和形状。
Pneumocystis may or may not be a fungus but are definitely black on GMS. They are flattened contact-lens–shaped organisms found in the alveoli (Figure 3.16). They are not visible on HE but are usually accompanied by a foamy pink exudate.
肺孢子菌可能是也可能不是真菌(译注:最近研究多认为真菌),但在GMS上肯定是黑色的。它们是在肺泡中发现的,呈扁平的隐形眼镜形状的病原体(图3.16)。它们在HE上不可见,但通常伴有泡沫状粉红色渗出物。
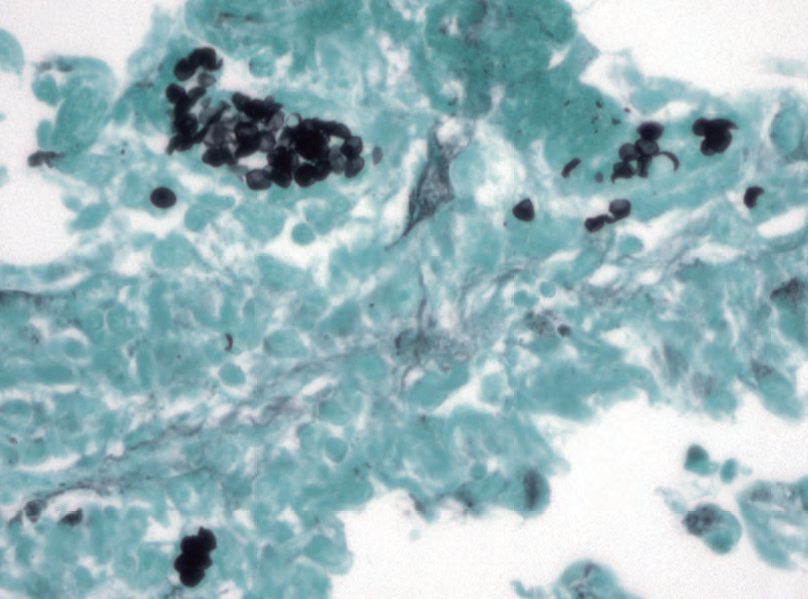
Figure 3.16. Pneumocystis. This photograph in the lung is taken at the same power as Figures 3.14 and 3.15. The organisms are stained with Gomori’s methenamine silver stain.
图3.16.肺孢子菌。这张肺部照片是以与图3.14和3.15相同的倍数拍摄的。这些病原体用Gomori六胺银染色剂染色。
3.4.2 细菌(Bacteria)
Most bacteria are not found by, or identified with, stains. This is because there is little more we could say than “Gram-positive cocci in clusters,” for example, which is pretty unhelpful without a culture. There are a few that are hard to culture and are best identified by stains.
Histologic evidence of Mycobacterium (causing tuberculosis and other diseases) is caseating granulomas. The organisms are not seen on HE and may be very sparse in an immunocompetent patient. The conventional stain is the acid-fast (AFB) stain, which leaves the tissue unstained, with occasional pink blush in some cell types, but stains mycobacteria a bright wine red (Figure 3.17). These are tiny scattered bacilli; you need to be at 40×, at least, to spot them. Scanning the entire slide at 40× for red lint is painful but necessary to rule out infection. If clinical suspicion is high but an AFB is negative, an auramine-rhodamine is a more sensitive fluorescent stain for tuberculosis.
大多数细菌不能通过染色而发现或识别。这是因为我们只能说“革兰氏阳性球菌群”之类的描述,例如,没有细菌培养是毫无帮助的。有一些很难培养,最好通过染色来识别。
分枝杆菌(引起结核病和其他疾病)的组织学证据是干酪样肉芽肿。这些微生物在HE上看不到,在免疫功能正常的患者中可能非常稀少。传统的染色法是抗酸(AFB)染色法,染色效果是组织不染色,某些细胞类型偶尔呈现粉红色,但分枝杆菌染成明亮的酒红色(图3.17)。它们是微小的分散的杆菌;你至少需要在40x才能发现它们。以40x扫描整个载玻片寻找红色线条是痛苦的,但必须排除感染。如果临床高度怀疑,但AFB阴性,可以使用对结核杆菌更敏感的金胺罗丹明(auramine-rhodamine)荧光染色。
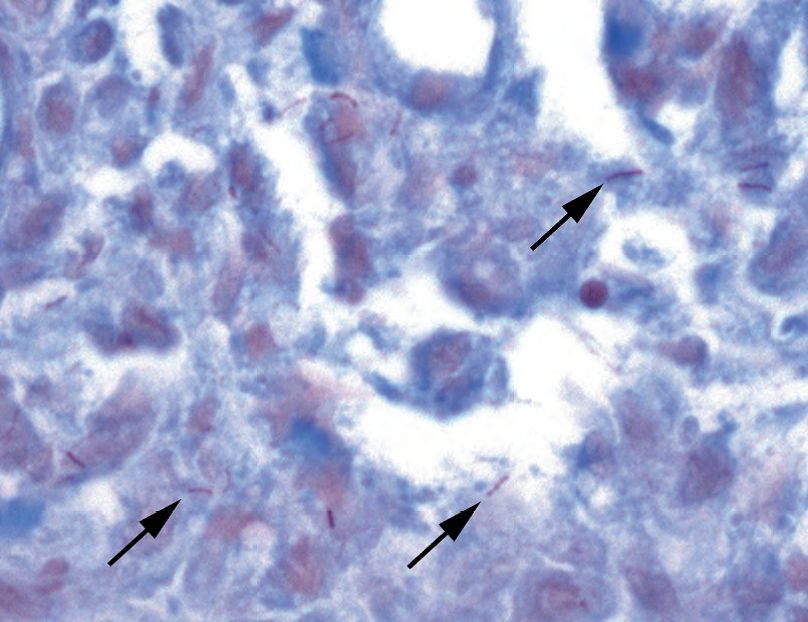
Figure 3.17. Mycobacteria on acid-fast bacteria stain. In this example, tiny wine-red rods are visible within the tissue (arrows).
图3.17.抗酸染色上的分枝杆菌。在本例中,组织内可见微小的酒红色杆状物(箭头)。
Mycobacterium avium-intracellulare causes infection in an immunocompromised patient. In these patients, the mycobacteria are eaten by macrophages and then multiply like crazy within the cells, giving the appearance of foamy macrophages. In the duodenum this can look just like Whipple’s disease, but a PAS stain will differentiate the two (histiocytes stuffed with cranberries in Whipple’s disease but with fine bacilli in M. avium-intracellulare infection). An AFB stain will also be positive.
鸟分枝杆菌引起免疫功能低下患者感染。在这些患者中,分枝杆菌被巨噬细胞吞噬,然后在细胞内疯狂繁殖,形成泡沫状巨噬细胞。在十二指肠中,这可能看起来像Whipple病,但PAS染色可以区分这两种疾病(Whipple病中的组织细胞充满蔓小红莓,但鸟分枝杆菌感染表现为组织细胞内细小杆菌)。AFB染色也呈阳性。
Helicobacter pylori is the most common cause of gastric ulcers. Histologically you should see a chronic inflammatory infiltrate in the stomach, with a little activity here and there (polys). Infection is more common in the antrum. On Diff-Quik or Giemsa stain, look in the areas of activity. If present, H. pylori will be in the pit lumens or at the surface in clusters of tiny (barely visible at 20×) seagull-shaped bacilli (Figure 3.18). Sometimes you will hear them called helicopters. This is a phonetic joke, not a visual one. They do not look like helicopters.
幽门螺杆菌(HP)是胃溃疡最常见的病因。组织学上,你应该看到胃内有慢性炎症细胞浸润,局部有少量活动性炎症(中性粒细胞)。感染多见于胃窦。在Diff-Quik或Giemsa染色上,观察活动性炎症区域。如果存在HP,胃小凹或胃黏膜表面可见微小的(20×几乎看不见)海鸥形状的杆菌形成小簇(图3.18)。有时你会听到他们叫直升机。这是一个语音笑话(译注:英文直升机与HP发音有点相似),不是视觉笑话。它们看起来不像直升机。
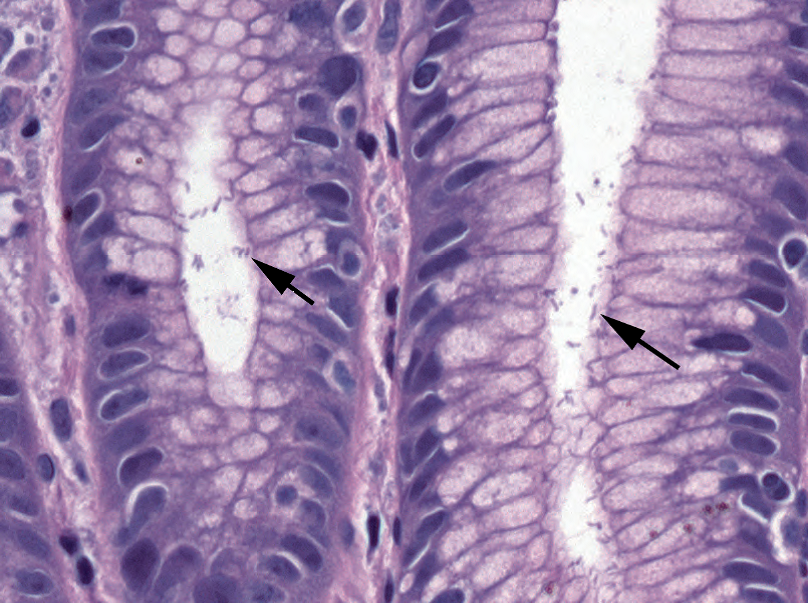
Figure 3.18. Helicobacter pylori. The bacilli are sometimes visible on hematoxylin and eosin stain, as seen here (arrows), in the pits of the gastric mucosa.
图3.18.幽门螺杆菌。HE染色有时可在胃粘膜的胃小凹中看到杆菌(箭头所示)。
Actinomyces, causing a puffball bacterial colony, is completely unremarkable in the tonsil but significant in endometrium, especially in the setting of an intrauterine device. The HE appearance is of a granular grey-purple cloud, sometimes filamentous, with no identifiable cells or structures (Figure 3.19).
放线菌,产生一种泡芙球状菌落,在扁桃体中完全不显著,但在子宫内膜中显著,尤其是在放置宫内节育器时。HE表现为颗粒性灰紫色云絮状,有时呈丝状,没有可识别的细胞或结构(图3.19)。
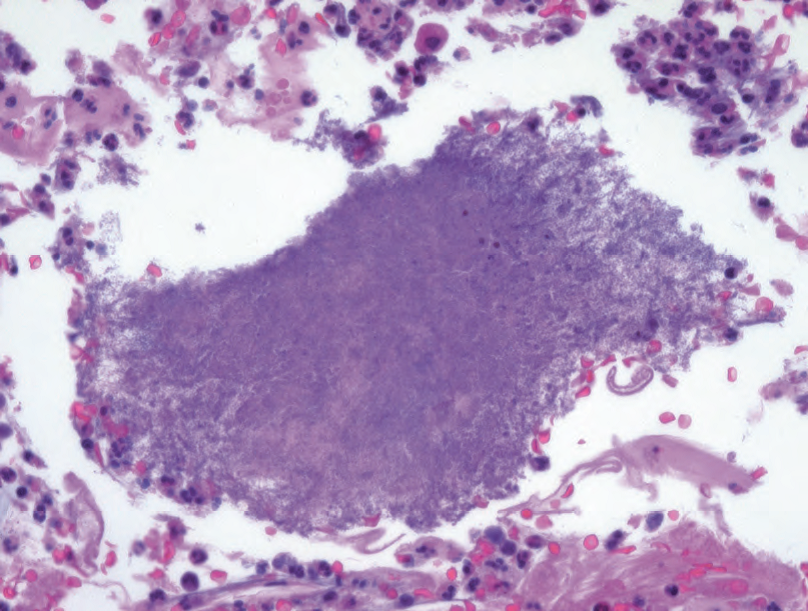
Figure 3.19. Actinomyces. This filamentous ball of organisms is easily overlooked, as it resembles fibrin.
图3.19.放线菌。这种病原体形成丝状球,很容易被忽视,因为它类似于纤维素。
3.4.3 病毒(Viruses)
Herpes simplex virus tends to cause extensive tissue damage and ulcers. It infects the epithelium, so look in the cells immediately adjacent to the ulcer. The cells become multinucleated, with the transformed nuclei molding into each other. The chromatin is entirely displaced by glassy nuclear inclusions (viral proteins), outlined by a dark rim of residual chromatin, as though the nucleus is being digested from the inside (Figure 3.20).
单纯疱疹病毒往往引起广泛的组织损伤和溃疡。它感染上皮,所以要观察紧邻溃疡的细胞。细胞变成多核,转化的细胞核相互嵌合(铸型)。染色质完全被毛玻璃样核内包含体(病毒蛋白)取代,残留染色质形成深染的环形边缘,就像细胞核从内部被消化一样(图3.20)。
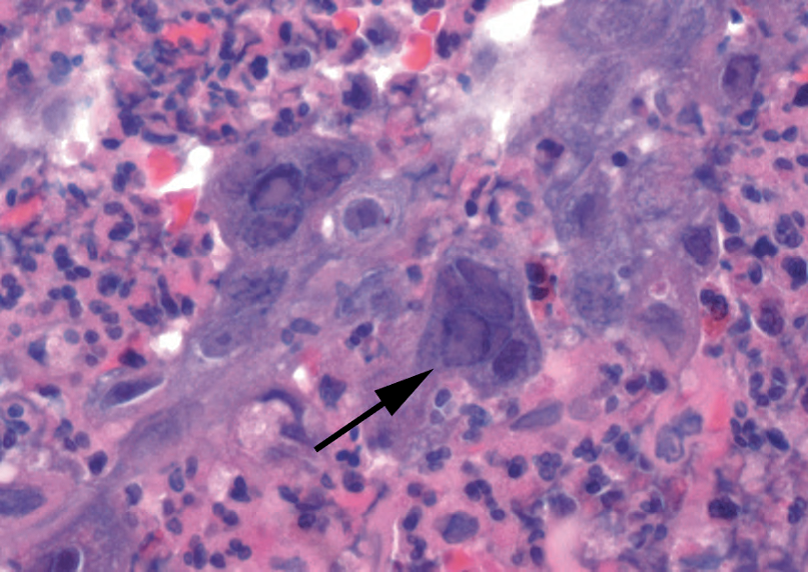
Figure 3.20. Herpesvirus. The classic nuclear changes include multiple molded nuclei with a peripheral rim of chromatin and a glassy inclusion nearly replacing the chromatin (arrow).
图3.20.疱疹病毒。典型的核变化包括多核镶嵌,染色质形成环形边缘,毛玻璃样包含体几乎取代了染色质(箭头)。
Cytomegalovirus can also cause ulcers but may infect tissue without obvious localizing damage. It infects epithelial, endothelial, and mesenchymal cells. In the case of an ulcer, look in the ulcer bed, not the periphery. The virus causes enlarged cells with large nuclei. The nuclei have a very characteristic inclusion; a dark dense round/oval inclusion surrounded by a pale halo, all within the nuclear membrane (Figure 3.21). The pale halo is not always entirely visible, so finding large dark round nuclei in a group of normal cells (nonneoplastic) should prompt you to consider cytomegalovirus. Immunostains help.
巨细胞病毒也可引起溃疡,但感染组织可能无明显局部损伤。它感染上皮细胞、内皮细胞和间叶细胞。如果是溃疡,要观察溃疡床,而不是周围。这种病毒导致细胞增大和核增大。细胞核具有非常典型的包含体;一种深染致密的圆形/椭圆形包含体,周围有淡染的空晕,这些结构全部位于核膜内(图3.21)。淡染的空晕并不总是完全可见,所以在一组正常细胞(非肿瘤细胞)中发现大的深染的圆形核应该促使你考虑巨细胞病毒。免疫染色有帮助。
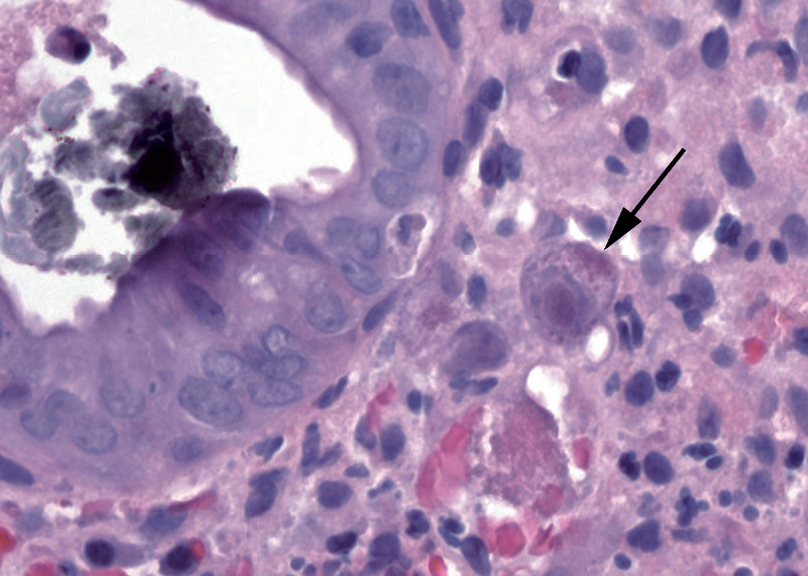
Figure 3.21. Cytomegalovirus. This infected endothelial cell in the gastrointestinal tract (arrow) shows the typical nuclear changes of cytomegalovirus, with a central reddish dense nuclear inclusion, surrounded by a clear halo and a rim of purple chromatin.
图3.21.巨细胞病毒。胃肠道中受感染的内皮细胞(箭头所示)显示巨细胞病毒典型的细胞核改变,中央有一个红色致密的核内包涵体,围绕着透明的光晕和一圈紫色的染色质边缘。
3.4.4 寄生虫(Parasites)
Giardia is a duodenal parasite that looks a little like a flounder with a long tail: it is kite shaped when viewed from above but a flat crescent from the side. It is found at the luminal surface of the villi and may not cause much inflammation. The parasites look very much like debris, but in a fortuitous cut you may see the “eyes,” which identify it. You will not see Giardia unless you look for it. It is related to Trichomonas, which you will see on pap smears.
贾第虫是一种十二指肠寄生虫,看起来有点像长尾的比目鱼:从上面看它是风筝形,但从侧面看它是扁平的新月形。在绒毛的腺腔表面发现,可能不会引起太多炎症。这种寄生虫看起来很像碎片,但在一个偶然发现的伤口中,你可能会看到“眼睛”从而识别它。除非你有意识地寻找,否则你不会看到贾第虫。它与滴虫有关,你可以在宫颈涂片上看到。
Cryptosporidium is another duodenal parasite that mainly infects the immunocompromised. The tiny round parasites line up along the brush border like clinging bubbles.
隐孢子虫是另一种十二指肠寄生虫,主要感染免疫功能低下者。这些微小的圆形寄生虫沿着刷状缘排列,就像粘在一起的泡泡。
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。
本站欢迎原创文章投稿,来稿一经采用稿酬从优,投稿邮箱tougao@ipathology.com.cn
相关阅读
 数据加载中
数据加载中
我要评论

热点导读
-

淋巴瘤诊断中CD30检测那些事(五)
强子 华夏病理2022-06-02 -

【以例学病】肺结节状淋巴组织增生
华夏病理 华夏病理2022-05-31 -

这不是演习-一例穿刺活检的艰难诊断路
强子 华夏病理2022-05-26 -

黏液性血性胸水一例技术处理及诊断经验分享
华夏病理 华夏病理2022-05-25 -

中老年女性,怎么突发喘气困难?低度恶性纤维/肌纤维母细胞性肉瘤一例
华夏病理 华夏病理2022-05-07






共0条评论