[导读] 原创: 乳腺癌研究与治疗
雌激素受体(ER)、孕激素受体(PR)和人类表皮生长因子受体2(HER2)的表达状态,对于指导乳腺癌患者的治疗决策至关重要。在日常工作中,ER、PR、HER2状态通常需要检测两次,即肿瘤穿刺活检诊断时、肿瘤完整切除手术后。
2019年2月13日,施普林格·自然旗下《乳腺癌研究与治疗》在线发表荷兰特文特大学、鹿特丹大学、澳大利亚墨尔本大学的研究报告,利用荷兰乳腺癌患者的真实世界个体水平数据,比较了肿瘤穿刺活检与肿瘤完整切除的ER、PR、HER2表达状态。
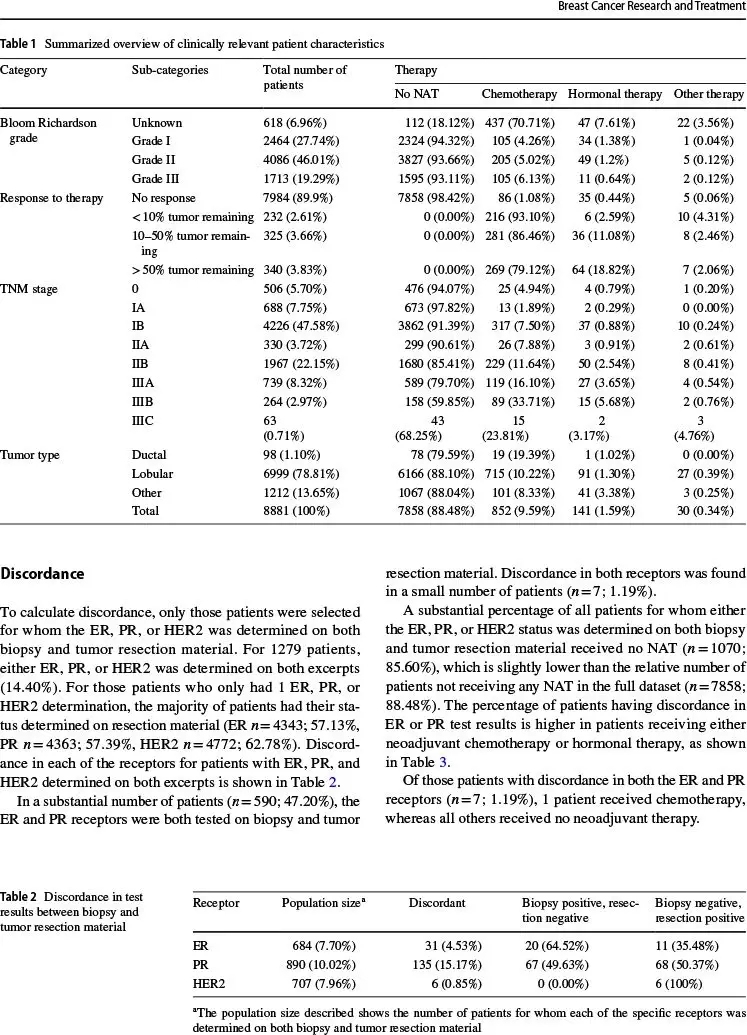
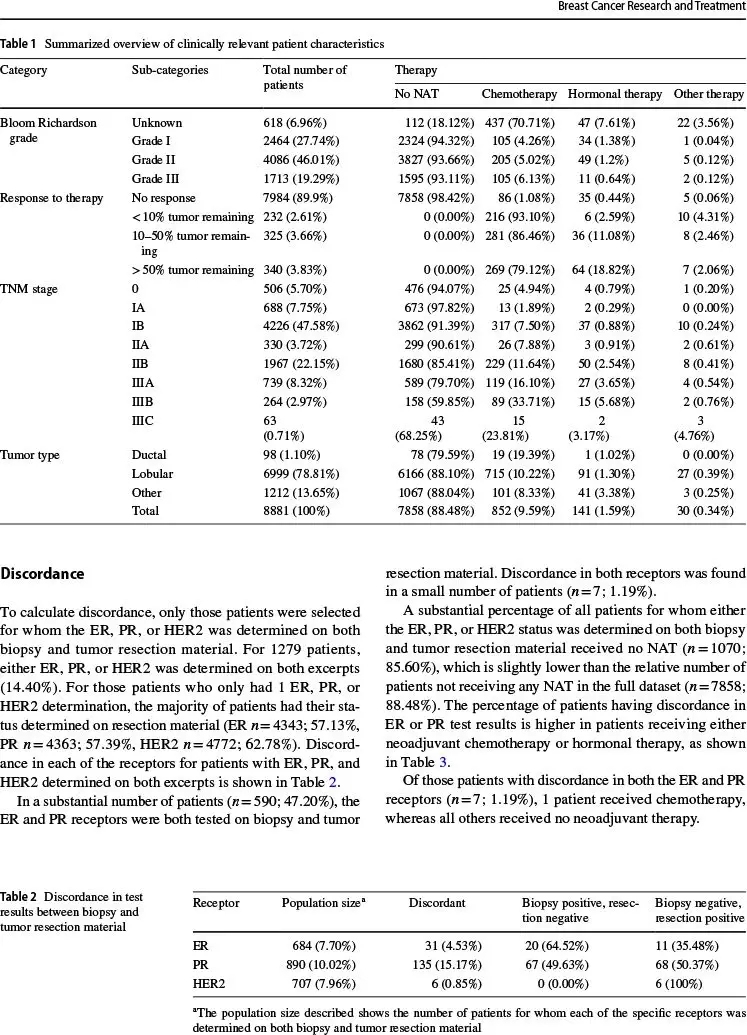
该研究对2016年1月12日~2018年1月1日荷兰病理登记中心1万1054例乳腺癌患者的病理报告进行回顾分析,对ER、PR、HER2表达状态的各种组合进行比较。通过针对ER、PR、HER2的多个逻辑回归模型,分析患者特征和肿瘤特征对检测结果的影响。
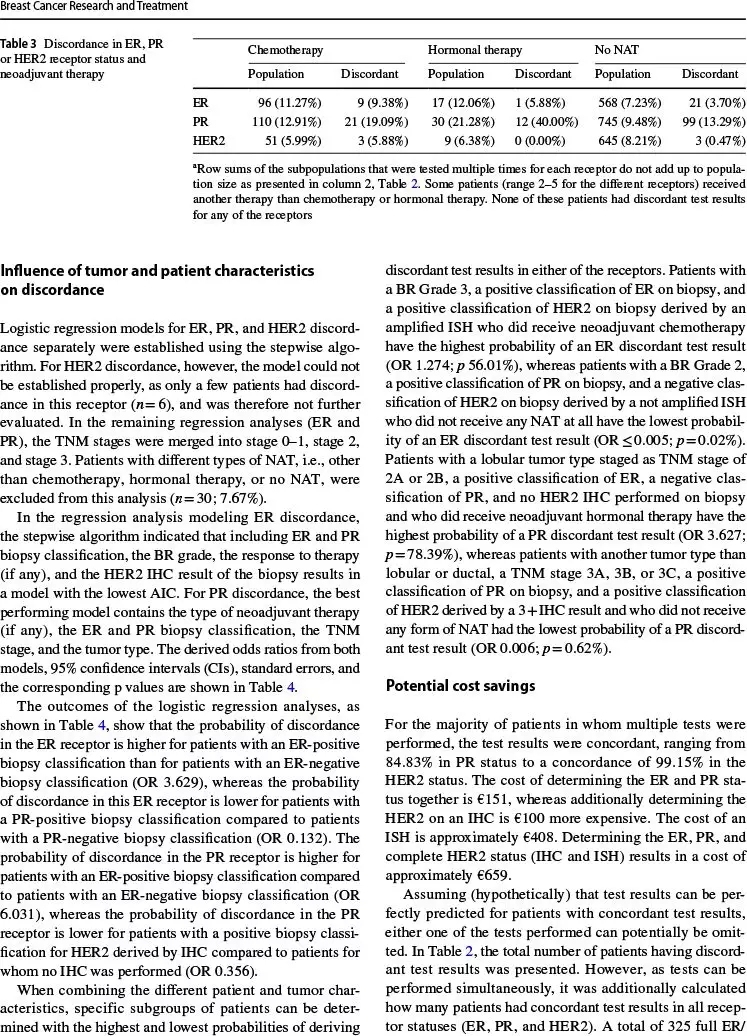
结果,仅1279例患者(14.4%)活检与切除的肿瘤组织均检测了至少一种受体(ER、PR、HER2),活检与切除的检测结果大多一致:
ER(916例,94.8%)
PR(1170例,86.7%)
HER2(881例,98.1%)
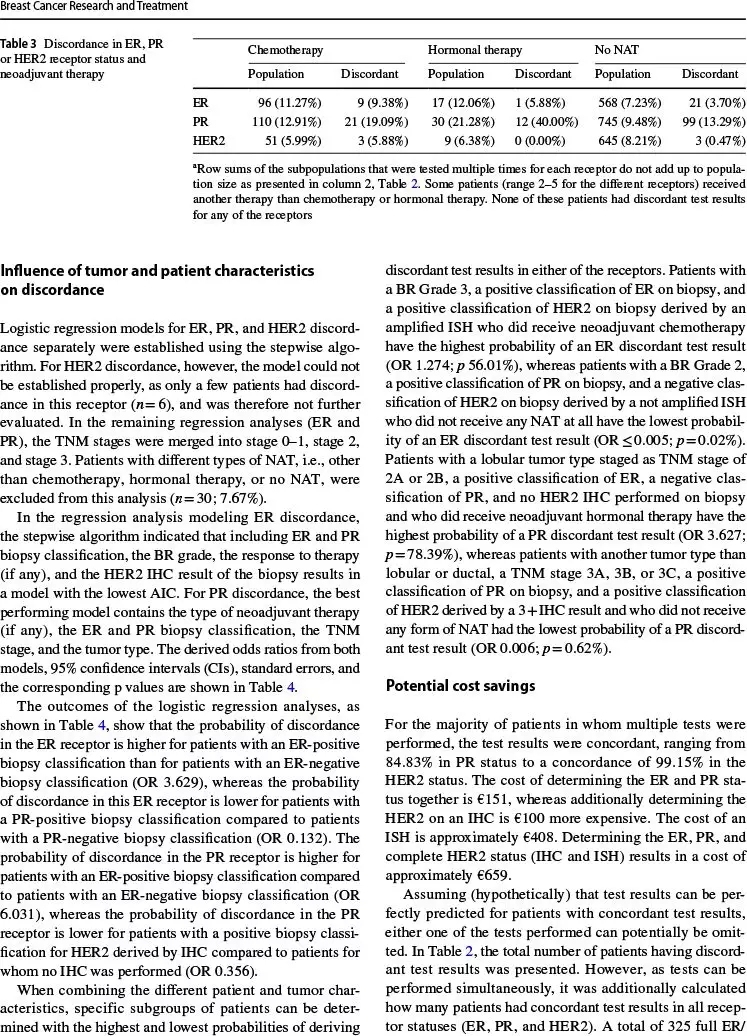
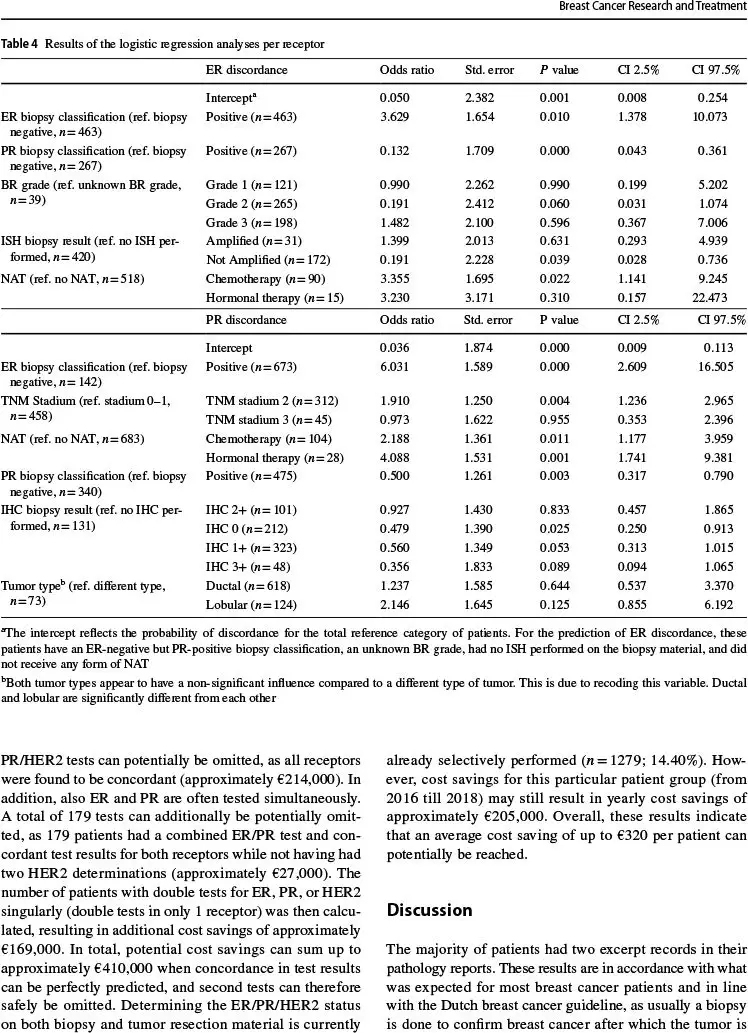
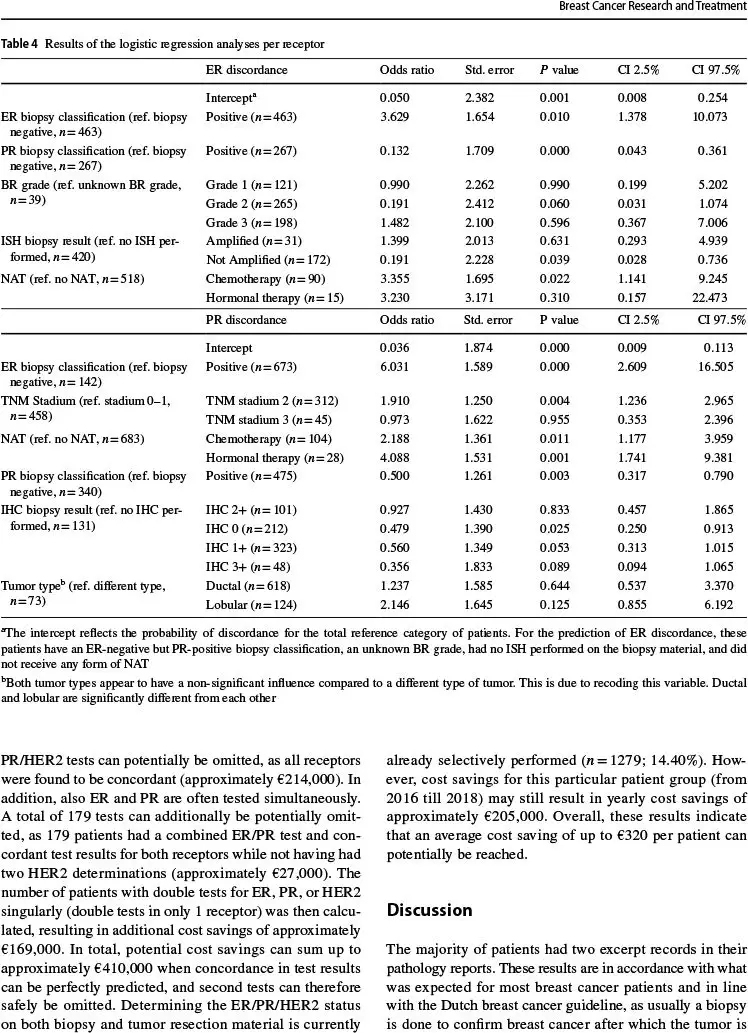
对于活检ER和HER2阳性而PR阴性、乳腺癌III级、术前新辅助治疗后残余肿瘤组织<10%的患者,ER检测结果不一致率最高(比值比:4.991,P=83.31%)。根据不同的患者特征和肿瘤特征,PR检测结果不一致率不同。
如果可以准确预测检测结果一致,那么可以节省多次检测费用,每年高达20万5000欧元。
因此,该研究结果表明,ER、PR、HER2的双次检测率仅14.4%,少于预计。对于接受双次检测的患者,初步诊断时肿瘤穿刺活检与手术治疗时肿瘤完整切除的ER、PR、HER2检测结果不一致率很低,尤其对于术前未接受任何形式新辅助治疗的患者,意味着对于这些乳腺癌患者或许可以免去大量重复检测。
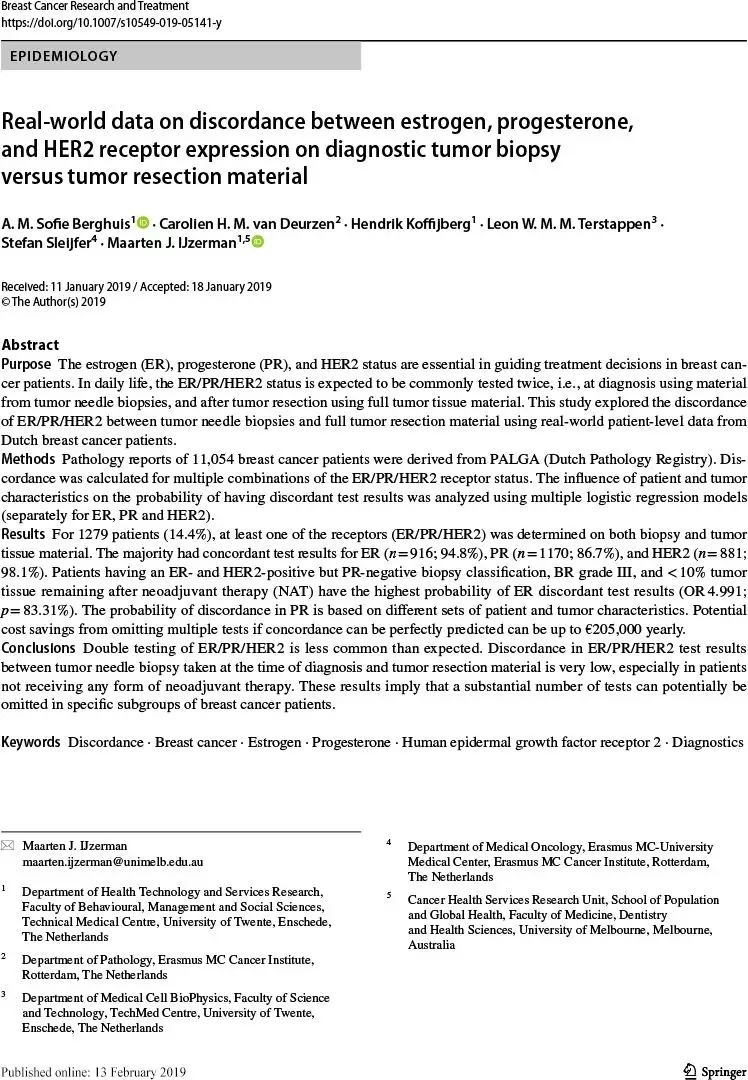
Breast Cancer Res Treat. 2019 Feb 13.
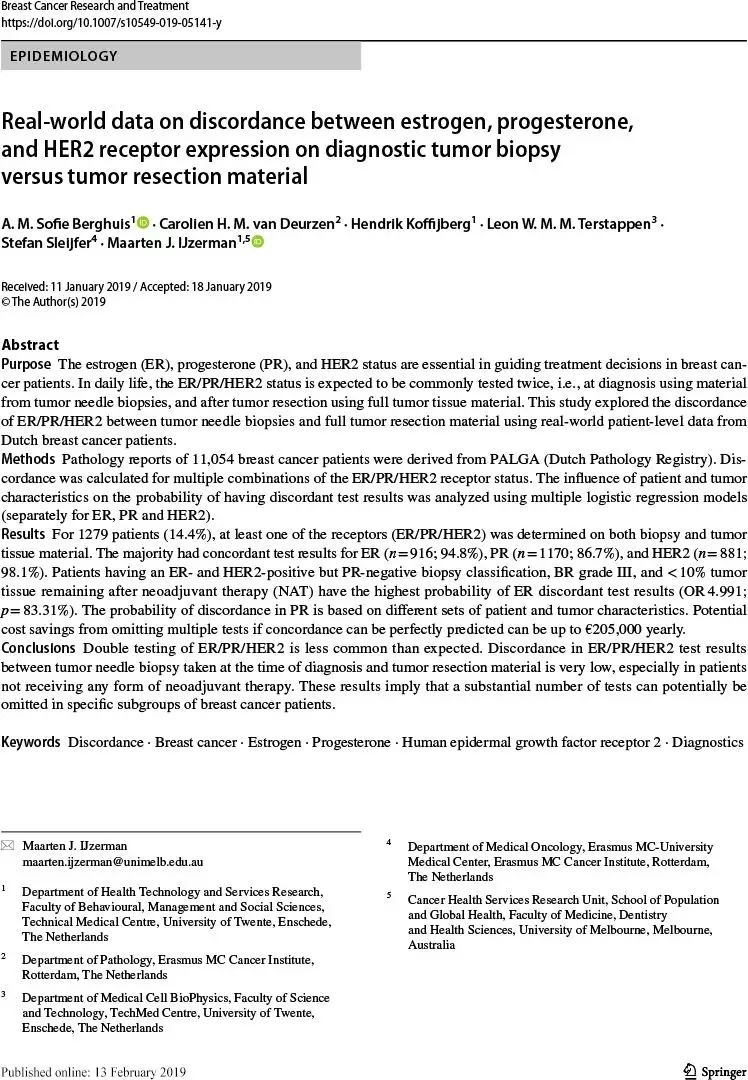
Real-world data on discordance between estrogen, progesterone, and HER2 receptor expression on diagnostic tumor biopsy versus tumor resection material.
A. M. Sofie Berghuis, Carolien H. M. van Deurzen, Hendrik Koffijberg, Leon W. M. M. Terstappen, Stefan Sleijfer, Maarten J. IJzerman.
University of Twente, Enschede, The Netherlands; Erasmus MC Cancer Institute, Rotterdam, The Netherlands; University of Melbourne, Melbourne, Australia.
PURPOSE: The estrogen (ER), progesterone (PR), and HER2 status are essential in guiding treatment decisions in breast cancer patients. In daily life, the ER/PR/HER2 status is expected to be commonly tested twice, i.e., at diagnosis using material from tumor needle biopsies, and after tumor resection using full tumor tissue material. This study explored the discordance of ER/PR/HER2 between tumor needle biopsies and full tumor resection material using real-world patient-level data from Dutch breast cancer patients.
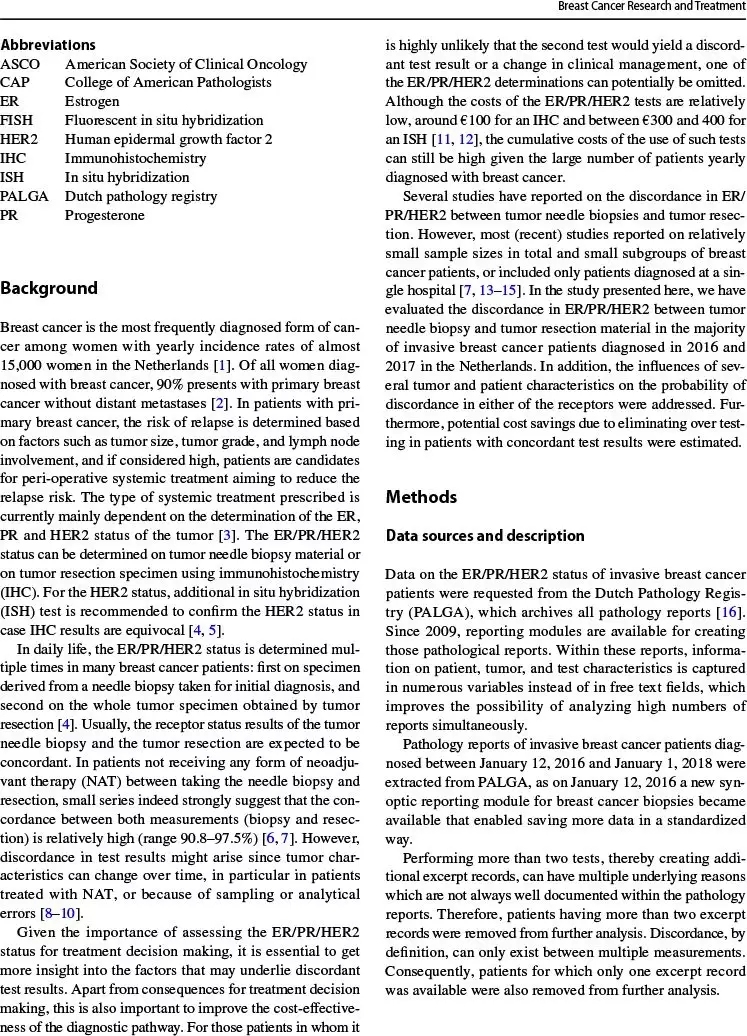
METHODS: Pathology reports of 11,054 breast cancer patients were derived from PALGA (Dutch Pathology Registry). Discordance was calculated for multiple combinations of the ER/PR/HER2 receptor status. The influence of patient and tumor characteristics on the probability of having discordant test results was analyzed using multiple logistic regression models (separately for ER, PR and HER2).
RESULTS: For 1279 patients (14.4%), at least one of the receptors (ER/PR/HER2) was determined on both biopsy and tumor tissue material. The majority had concordant test results for ER (n=916; 94.8%), PR (n=1170; 86.7%), and HER2 (n=881; 98.1%). Patients having an ER- and HER2-positive but PR-negative biopsy classification, BR grade III, and <10% tumor tissue remaining after neoadjuvant therapy (NAT) have the highest probability of ER discordant test results (OR4.991; p=83.31%). The probability of discordance in PR is based on different sets of patient and tumor characteristics. Potential cost savings from omitting multiple tests if concordance can be perfectly predicted can be up to €205,000 yearly.
CONCLUSIONS: Double testing of ER/PR/HER2 is less common than expected. Discordance in ER/PR/HER2 test results between tumor needle biopsy taken at the time of diagnosis and tumor resection material is very low, especially in patients not receiving any form of neoadjuvant therapy. These results imply that a substantial number of tests can potentially be omitted in specific subgroups of breast cancer patients.
KEYWORDS: Discordance Breast cancer Estrogen Progesterone Human epidermal growth factor receptor 2 Diagnostics
DOI: 10.1007/s10549-019-05141-y














共0条评论