外科病理学实践:诊断过程的初学者指南 | 第16章 宫颈和阴道(Cervix and Vagina)
第16章 宫颈和阴道(Cervix and Vagina)
Cervical biopsies are common and nearly always performed for the purpose of evaluating squamous or glandular dysplasia. Usually the patient will have a history of an abnormal Pap test or a prior abnormal biopsy finding. Correlation with cytology is nice, but lesions can be focal and/or transient, so perfect agreement is not required.
宫颈活检是常见标本,几乎总是为了评估鳞状或腺体异型增生而进行的。患者常有宫颈细胞学异常病史或先前的活检已经发现异常。与细胞学的相关性很好,但病变可能是局灶性和/或一过性,因此并不要求活检与细胞学完全一致。
There are several types of specimens. The smallest is usually the endocervical curettage. This is meant to be a sampling of the endocervix, and so should contain endocervical (columnar) mucosa. These tissue scrapings may have tiny and maloriented fragments, and the tissue can be spread out over a wide area.
有几种类型的标本。最小的通常是宫颈管搔刮术。这是对宫颈内膜的取样,因此应包含宫颈内膜(柱状)粘膜。搔刮获取的这些组织可能有微小的、方向不佳的碎片,并且组织包埋可能分散到很广泛的区域。
If a lesion is seen by the clinician on colposcopy, there may be a cervical biopsy performed, which is a crescent-shaped chunk taken out of the cervix. This tiny specimen is uninked and unoriented. A high-grade lesion requires a cone biopsy, where the transition zone is taken out in a conical fragment with the goal of completely excising the lesion. The cone biopsy may be done with cautery (loop electrosurgical excision procedure) or blade (cold-knife cone). The endocervical margin should be identified and inked to make sure the lesion is not extending up into the canal where it cannot be seen or sampled. The ectocervical margin is also inked, but a positive ectocervical margin is unusual.
如果临床医生在阴道镜检查中发现病变,可能会进行宫颈活检,即从宫颈钳取一块月牙形组织块。这种微小标本不会涂抹墨汁,也没有方向。高级别病变需要锥形活检,在切除的锥形组织片段中包括移行区,目的是完全切除病变。锥形活检可采用电灼法(电刀环切)或刀片法(冷刀锥切)进行。应识别子宫颈管切缘,并涂抹墨汁,以确保病变未延伸到先前活检时无法看到或无法取样的子宫颈管内。外子宫颈切缘也涂抹墨汁,但宫颈外切缘呈阳性是少见的。
正常组织学(Normal Histology)
The cervix is covered by a nonkeratinized squamous epithelium that merges into the surrounding vaginal wall. The squamous cells may be full of glycogen and have a plump cleared-out cytoplasm (see Figure 4.8B). In postmenopausal women, the epithelium may become thin and atrophic, with an immature look.
宫颈被覆非角化鳞状上皮,并与周围阴道壁融合。鳞状细胞可能充满糖原,胞质丰满、透明(见图4.8B)。绝经后妇女的上皮可能变薄萎缩,外观不成熟。
The transition zone represents an abrupt transition to mucous-secreting columnar and glandular epithelium and may be located at the os or within the endocervical canal. Irritation or inflammation at the transition zone may lead to acute and/or chronic inflammation and squamous metaplasia overlying the glandular mucosa. This state is so universal that “chronic cervicitis and squamous metaplasia” is synonymous with normal. Squamous metaplasia, by definition, can only occur at or above the transition zone (Figure 16.1), and so mentioning it confirms that the transition zone was sampled. If you see no endocervical component at all, the specimen is simply “benign squamous mucosa.”
移行区代表鳞状上皮向分泌粘液的柱状上皮(腺上皮)的突然过渡,可能位于子宫颈外口或子宫颈管内。移行区受刺激或炎症可能导致腺上皮粘膜发生急性和/或慢性炎症和鳞状化生。这种情况非常普遍,所以“慢性宫颈炎和鳞状化生”是正常表现。根据定义,鳞状化生只能发生在移行区或其上方(图16.1),因此在报告中记录鳞状化生,说明可以确认标本中含有移行区。如果你根本看不到宫颈内膜成分,标本仅仅是“良性鳞状粘膜”。

Figure 16.1. Squamous metaplasia at the transition zone. Mature squamous epithelium is seen to the right of the arrow, and squamous metaplasia is seen to the left. In squamous metaplasia, the nuclei may be larger and more immature appearing and the cytoplasm more dense.
图16.1 移行区鳞状化生。箭头右侧可见成熟鳞状上皮,左侧可见鳞状化生。在鳞状化生中,细胞核可能较更大,较不成熟,细胞质较致密。
Endocervical glands are branching and complex glands that are pale with a dark outline due to the large cytoplasmic mucin vacuole pushing aside a small crescent-shaped nucleus (Figure 16.2). Fragments of glands on endocervical curettage may have a papillary or inside-out look, which is not significant. Squamous metaplasia may fill up and replace glands and must be distinguished from invasive cancer. Crowding of otherwise benign-looking glands is not a feature of concern, as it is in the endometrium.
子宫颈管腺体是一种分支状复杂的腺体。由于细胞质含有大的粘液空泡,把小的细胞核推向一侧形成新月形,因此低倍镜下呈现淡染区和深染轮廓(图16.2)。宫颈管搔刮术中,腺体碎片可能呈现乳头状或内外倒置的外观,这种现象没有特殊意义。鳞状化生可能填满并取代腺体,必须与浸润性癌区分开来。其他方面表现良性的腺体但显得拥挤,并不值得关注,正如子宫内膜腺体所见。
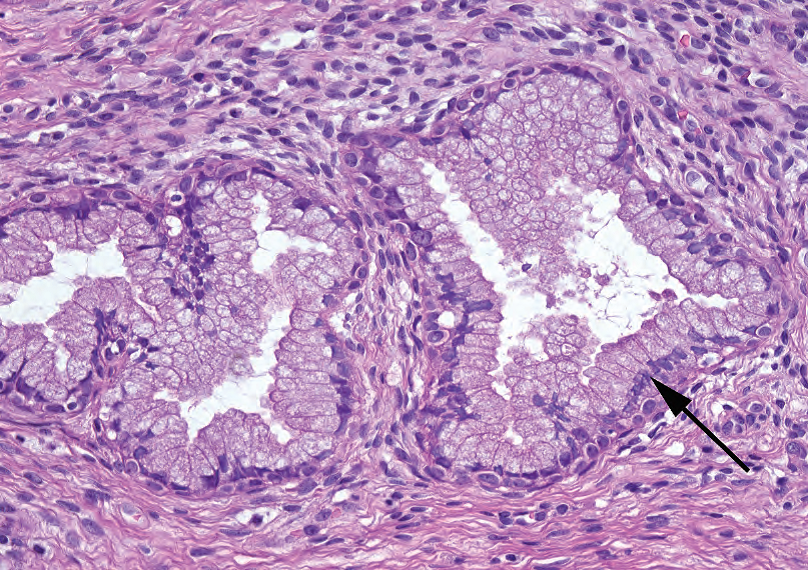
Figure 16.2. Endocervical glands. Normal endocervical glands are composed of tall columnar cells with apical mucin and small basal nuclei (arrow).
图16.2 子宫颈管腺体。正常的宫颈腺体由高柱状细胞组成,胞质顶端为粘液,核小,位于基底(箭头)。
The cervical stroma is very fibrotic (as you will find when cutting through one), so it looks pink and spindly. There are a variety of normal cysts and glandular proliferations that may occur within the stroma.
宫颈间质明显纤维化(你切割时会感受到),因此呈粉红色且梭形。间质内可能有多种正常囊肿和腺体增殖。
宫颈管搔刮术的观察方法(The Approach to the Endocervical Curettage)
First look at the slide on the tray, and circle a single level of the tissue—it may be spread out over a wide area, but may be duplicated several times on the same slide. At low power, look for fragments of squamous epithelium and endocervical glands. The presence or absence of each is noted in the diagnosis. There may be a fair amount of background mucus (stringy pale pink amorphous substance) and inflammation. Concentrate on the actual epithelial fragments, if there are any. A smear of scattered endocervical cells (columnar cells with apical mucin) may be all you get, but ideally there are fragments of squamous epithelium to evaluate. These are evaluated by the same criteria as the biopsy, described next.
首先,肉眼观察托盘上的切片,把组织范围划一个圈,它可能分散在很广泛的区域,也可能在同一张切片重复放置了几片组织。低倍镜下,寻找鳞状上皮和宫颈腺体的片段。要在诊断报告中注明上述两种成分是否存在。可能有相当数量的背景粘液(丝状淡粉色无定形物质)和炎症。重点观察真实的上皮片段,如果有。切片上可能只有分散的宫颈内膜细胞(带有顶端粘液的柱状细胞),但理想情况下会有鳞状上皮片段进行评估。其评估方法和标准,与活检相同,如下文所述。
活检标本的观察方法(The Approach to the Biopsy)
On low power, first survey the squamous epithelium and the endocervical glands to look for areas that stand out as being more disorganized, darker, denser, or more inflamed than other areas. This applies to the squamous epithelium as well as to individual endocervical glands. Any suspicious area should be studied at higher magnification to look for the following:
在低倍镜下,首先检查鳞状上皮和宫颈腺体,寻找比其他区域更混乱、更深染、更密集或更重炎症的区域。这适用于鳞状上皮和单个宫颈腺体。应在更高倍研究任何可疑区域,以查找以下情况:
Low-grade squamous intraepithelial lesion (LSIL; cervical intraepithelial neoplasia grade 1 [CIN1])
低度鳞状上皮内病变(LSIL;宫颈上皮内瘤变1级[CIN1])
Low-grade squamous intraepithelial lesion is a viral cytopathic effect that affects primarily the upper cell layers of the epithelium.
LSIL是一种病毒性细胞病变,主要影响上皮的上层细胞。
The cells have pleomorphic, wrinkled, hyperchromatic nuclei with a perinuclear cleared halo; these are called koilocytes. Binucleation is common (Figure 16.3).
细胞有多形性、皱缩、深染的细胞核,核周有透明空晕;这些称为挖空细胞。双核常见(图16.3)。
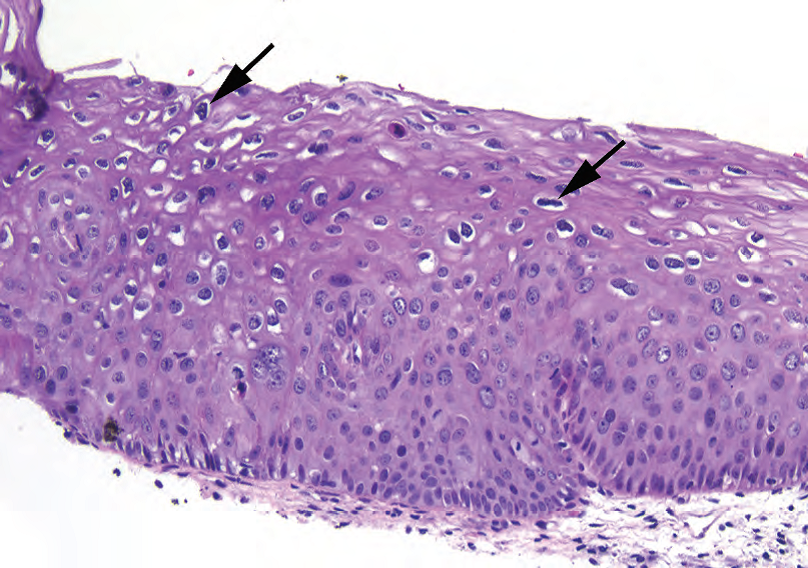
Figure 16.3. Low-grade squamous intraepithelial lesion. The hallmark of low-grade squamous intraepithelial lesion is the koilocyte, which is a squamous cell with HPV viral cytopathic effect. The nuclei are hyperchromatic (dark) and raisinoid (crinkly; see arrows), with a surrounding clear halo in the cytoplasm. Other good features include superficial nuclei that are larger than the nuclei below them and binucleated cells.
图16.3 LSIL。LSIL的标志是挖空细胞,它是HPV病毒导致的细胞病变。细胞核深染(暗)和葡萄干样(皱缩;箭),细胞质中有周围透明空晕。其他良好的诊断特征包括表层细胞核大于下方细胞核,和双核细胞。
It can look haphazard at low power, but the basal layer should be maintained, and mitoses should not be higher than the lower one third.
在低倍镜下,它看起来杂乱,但基底层应保持不变,核分裂位置不应高于上皮全层的下三分之一(译注:即,核分裂象局限于上皮的下1/3层)。
High-grade squamous intraepithelial lesion (HSIL; CIN2–3)
高度鳞状上皮内病变(HSIL;CIN2-3)
High-grade squamous intraepithelial lesion is a persistence of immaturity along with dysplastic changes. Essentially, the basal cells are becoming “immortalized,” like a cancerous cell, and are not maturing and differentiating as they should.
HSIL是一种持续存在的不成熟的异型增生改变。本质上,基底细胞变得“永生”,就像癌细胞一样,理应成熟和分化,却没有成熟和分化。
The overall impression is of a denser and darker epithelium due to the high nuclear/ cytoplasmic (N/C) ratios.
由于高核/质(N/C)比,总体印象是上皮更致密、更深染。
Atypia is seen in all cell layers, from the bottom up. The nuclei may not be as large or as bizarre as LSIL but are uniformly crowded, enlarged, and hyperchromatic with clumped chromatin and irregular membranes (boulder nuclei), and mitoses are present in the upper two thirds (Figure 16.4).
从下到上,所有细胞层均存在异型性。细胞核增大或奇异程度可能不如LSIL,但呈现均匀一致的拥挤、增大、深染伴粗块状染色质和核膜不规则(大圆石样核),上2/3层出现核分裂象(图16.4)。
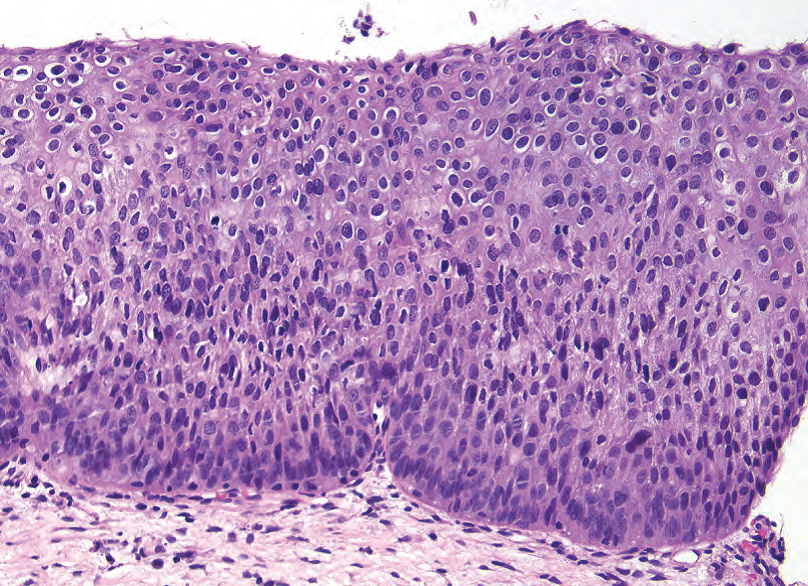
Figure 16.4. High-grade squamous intraepithelial lesion. In a high-grade lesion, paradoxically, the nuclei may not look as abnormal as in low-grade squamous intraepithelial lesion. The hallmark of highgrade squamous intraepithelial lesion is a persistence of immature-appearing cells throughout the epithelium. The nuclei are hyperchromatic and may have slightly irregular nuclear outlines, but the most striking feature at low power is the high nuclear/cytoplasmic ratios present from top to bottom.
图16.4 HSIL。矛盾的是,在HSIL中,细胞核异常程度可能不如LSIL。HSIL的特征是上皮内持续存在未成熟细胞。细胞核深染,核轮廓可能稍不规则,但在低倍镜下最显著的特征是从上到下呈现高核/质比。
CIN2 may show maturation at the surface or overlying LSIL.
CIN2可能在表面成熟或表面覆盖LSIL。
CIN3 shows full-thickness immaturity and atypia.
CIN3显示全层不成熟和异型性。
HSIL can grow into endocervical glands, which should be mentioned in the diagnosis.
HSIL可生长进入宫颈腺体中,诊断时应提及(译注,即,累及腺体)。
Do not confuse HSIL with immature squamous metaplasia, which has the following characteristics:
不要将HSIL与未成熟鳞状化生混淆,后者具有以下特征:
Well-defined cell borders and low N/C ratios
清晰的细胞边界和低N/C比
The “boiling mud” look (Figure 16.5)
“沸腾的泥浆”外观(图16.5)
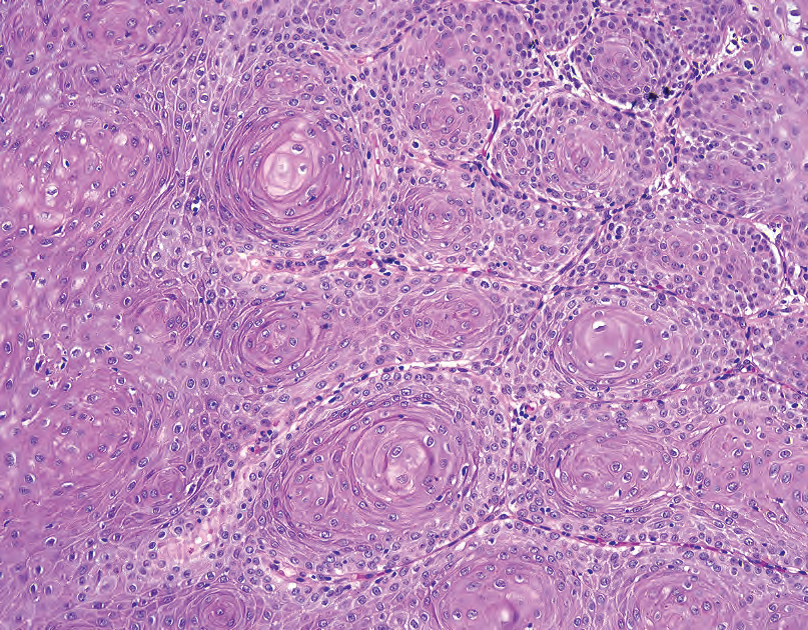
Figure 16.5. Immature squamous metaplasia. A tangential cut of squamous metaplasia can look like a lesion. However, this pattern of concentric whorls of cells with central pools of pink cytoplasm (resembling the boiling mud puddles of Yosemite) is typical of benign squamous metaplasia.
图16.5 未成熟鳞状化生。鳞状化生的斜切面看起来像病变。然而,这种细胞同心圆旋涡状模式和中心粉红色细胞质池(类似于约塞米蒂沸腾的泥坑)是良性鳞状化生的典型特征。
Usually pinker than HSIL
通常比HSIL更粉红
irds-egg nuclei (smooth, round, with even chromatin)
鸟卵核(光滑、圆形,染色质均匀)
Surface mucin or columnar layer
表面残留胞质粘液或柱状细胞层
In very tough cases, the two can be differentiated by Ki67 and p16. Ki67 should be positive only in the basal layer in metaplasia, and p16, a marker for human papillomavirus infection, should be negative (or at most, focal).
在非常困难的情况下,可以通过Ki67和p16来区分HSIL与未成熟鳞化。Ki67应当仅在化生的基底层呈阳性,而p16应为阴性(或最多为局灶性)。
反应性改变(Reactive Changes)
Be wary of calling an SIL in the context of extensive acute inflammation (neutrophils). Reactive changes include the following:
在广泛急性炎症(中性粒细胞)的情况下,不要轻率地诊断鳞状上皮内病变。反应性改变包括以下方面:
Regularly spaced nuclei with prominent nucleoli, homogeneous size, and smooth contours (Figure 16.6)
核分布规则,核仁明显,大小均匀,轮廓光滑(图16.6)
Maturing upper layers without atypia
上层成熟,无异型性
Spongiotic edema
海绵状水肿
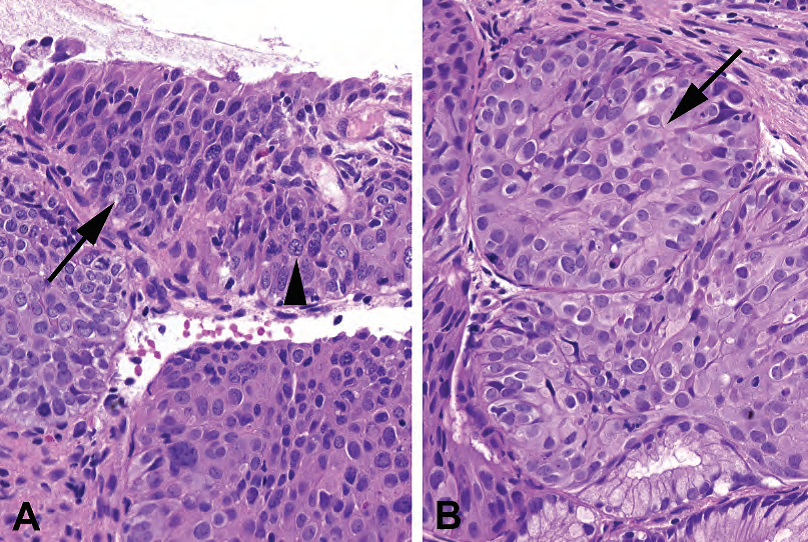
Figure 16.6. Dysplasia versus reactive changes. (A) In this example of high-grade squamous intraepithelial lesion, the dysplastic nuclei are irregularly shaped and appear to interlock together like stones in a wall (arrow). The quality of the chromatin is characteristic as well; it is dark and granular. Occasional nucleoli are visible (arrowhead), but they are surrounded by clumpy chromatin within the nucleus. (B) In reactive changes, the nuclei may be enlarged, but each nucleus remains smooth and oval in shape. The chromatin has a fine, even texture and is pale in color compared to the dysplastic cells in A. Small dense nucleoli are visible in many of the cells (arrow).
图16.6 异型增生与反应性改变。(A)HSIL,异型增生的细胞核形状不规则,看起来像石墙上交错在一起的大圆石(箭)。染色质的质地也有特征性;它是深染颗粒状的。偶尔可见核仁(箭头),但它们被细胞核内的粗块状染色质所包围。(B)在反应性改变中,细胞核可能增大,但每个细胞核保持光滑和椭圆形。与图(A)中的异型增生细胞相比,染色质细腻均匀,颜色淡染。在许多细胞中可见小而致密的核仁(箭)。
浸润性鳞状细胞癌(Invasive Squamous Cell Carcinoma)
In the case of extensive HSIL (which is functionally carcinoma in situ), you should carefully search for evidence of invasion. As with squamous carcinoma in the skin or oropharynx, identifying invasion can be difficult and depends on multiple features. Features of invasion are similar to those in other sites:
对于广泛性HSIL(其功能方面达到原位癌程度),应仔细寻找浸润证据。与皮肤或口咽鳞状细胞癌一样,可能难以识别浸润,并且取决于多种特征。浸润特征与其他部位类似:
Deep keratinization
深部角化
Large nucleoli
大核仁
Blurred or sawtooth interface between epithelium and stroma (Figure 16.7)
上皮和间质之间的界面模糊或锯齿状(图16.7)
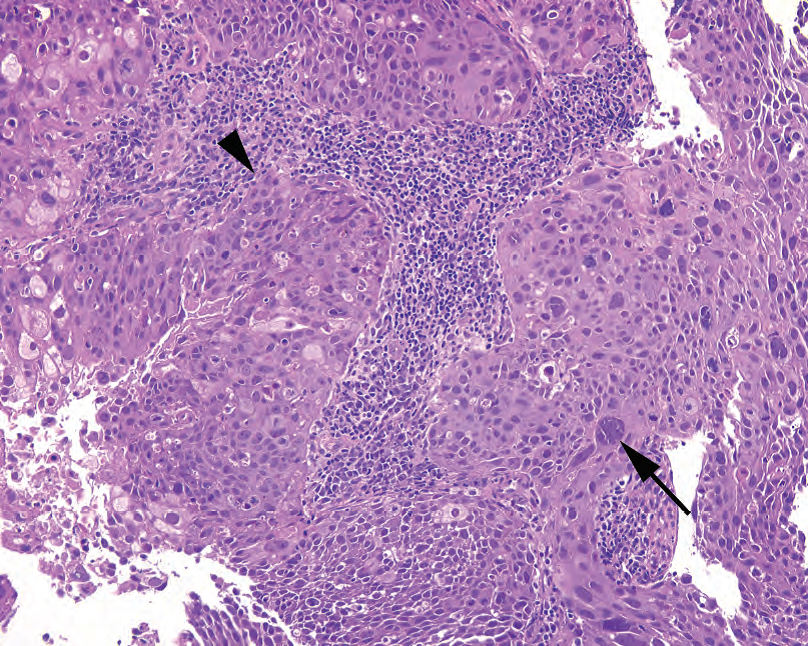
Figure 16.7. Invasive squamous cell carcinoma. Broad fronts of cells push into the stroma of the cervix, and at the leading edge there is a ragged border with individual infiltrating cells (arrowhead). Occasional huge and pleomorphic cells are visible (arrow).
图16.7 浸润性鳞状细胞癌。宽大的细胞前沿推挤进入宫颈间质,在前缘处呈现参差不齐的边界并有单个浸润细胞(箭头)。偶见巨大的多形性细胞(箭)。
Loss of palisading basal layer
基底层不再呈栅栏状排列
Desmoplastic response within stroma
间质内促结缔组织增生反应
Invasion to a depth of less than 3 mm is considered microinvasion and has a better prognosis.
浸润深度小于3mm视为微小浸润,预后较好。
The differential diagnosis for invasion includes pseudoepitheliomatous hyperplasia, glandular involvement by HSIL, and placental site nodules. HSIL has a tendency to crawl down into endocervical glands, much like squamous metaplasia does. Although this is important and should be mentioned, it must be differentiated from invasion. Clues include remnants of columnar epithelium, a smooth rounded contour to the gland, and the lack of individual cells in the stroma.
浸润的鉴别诊断包括假上皮瘤样增生、HSIL累及腺体和胎盘部位结节。HSIL有向下爬行进入宫颈腺体的倾向,其生长方式很像鳞状化生。虽然这很重要,报告中应该提到,但必须与浸润区分开来。诊断线索包括柱状上皮的残余、光滑的圆形腺体轮廓以及间质中缺乏单个细胞。
A placental site nodule is a remote remnant of pregnancy—aggregates of intermediate trophoblastic cells that have large single nuclei that can look atypical, found in hyaline nodules. Their pink cytoplasm and atypical cells may remind you of deep invasive keratinizing cells (Figure 16.8). However, the cell borders should be less well defined than squamous nests, and the nuclei show bizarre degenerative atypia—large, dark, and smudgy (meaning, little chromatin detail) nuclei without nucleoli.
胎盘部位结节是妊娠中期滋养层细胞聚集的远期残余物,这些细胞有大的单核,看似异型性,见于透明结节。它们粉红色的细胞质和非典型细胞可能让人想起深部浸润性角化细胞(图16.8)。然而,细胞边界应不如鳞状细胞巢清晰,细胞核表现出奇异形退变性非典型性——大、深染、污浊(意味着染色质细节看不清),无核仁。
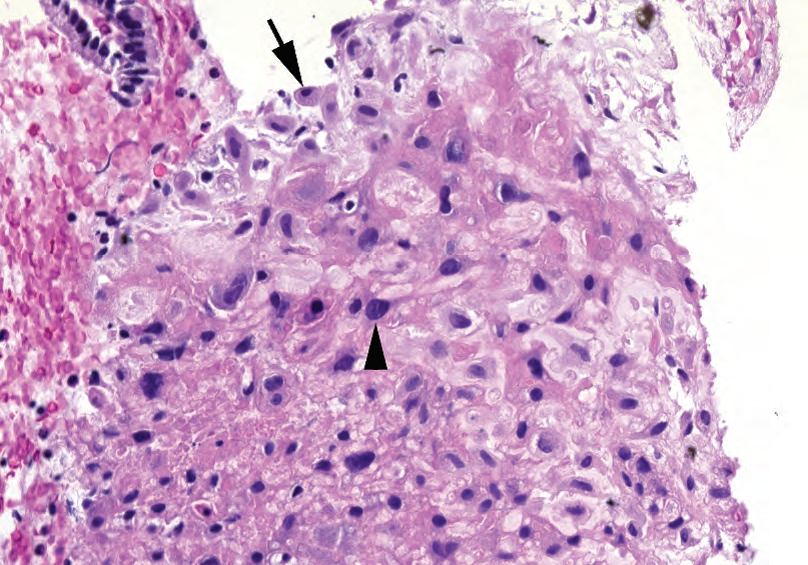
Figure 16.8. Placental site nodule, cervix. Although the dark nuclei and pink cytoplasm are concerning for squamous cell carcinoma, the nuclei are predominantly small and oval, with a few large nuclei visible (arrowhead). These large cells have dark but smudgy (blurred or indistinct) chromatin, without the chunky texture seen in HSIL (see Figure 16.6) and do not have the nuclear membrane irregularity of invasive squamous cell carcinoma (see Figure 16.7). The final clue is what appears to be a decidualized cell at the periphery (arrow).
图16.8 宫颈的胎盘部位结节。尽管核深染、胞质粉红色令人担心鳞状细胞癌,但核主要为小而椭圆形,只有少数大核(箭头)。这些大细胞有深染、污浊的染色质(模糊或看不清),不像HSIL中的粗块状染色质(见图16.6),也不像浸润性鳞状细胞癌的核膜不规则(见图16.7)。最后一条线索是在外围出现的蜕膜化细胞(箭)。
杂七杂八的良性实体(Miscellaneous Benign Entities)
Endocervical polyps have fibrotic (spindly) stroma with a polypoid shape and normal endocervical glands or epithelium. The may have cysts, inflammation, or tubal metaplasia (luminal cilia).
宫颈内膜息肉有纤维性(梭形)间质,呈息肉状,宫颈内膜腺体或上皮都是正常的。患者可能有囊肿、炎症或输卵管化生(管腔面有纤毛)。
Nabothian cysts are large dilated mucous-filled glands, lined with columnar epithelium. Tunnel clusters are lobular groups of complex branching glands (cystic or tubular), with benign columnar epithelium.
宫颈腺体囊肿(纳氏囊肿)是一种大型扩张的充满粘液的腺体,内衬柱状上皮。隧道状腺簇是由复杂分支腺体(囊性或管状)组成的小叶状分布的腺体群,具有良性柱状上皮。
Microglandular hyperplasia is associated with oral contraceptive pills. It looks like a proliferation of small back-to-back glands lined with cuboidal or columnar cells with mucin vacuoles (Figure 16.9). The low-power impression is that of a cribriform architecture, but the glands should still appear overall pale and pink, in contrast to the dark blue adenocarcinoma in situ (AIS) (discussed later).
微腺体增生与口服避孕药有关。它看起来像是小的背靠背腺体的增殖,排列着立方形或柱状细胞,细胞质有粘液空泡(图16.9)。低倍镜下为筛状结构,但腺体仍应整体呈淡粉色,与深蓝色原位腺癌(AIS)形成对比(稍后讨论)。
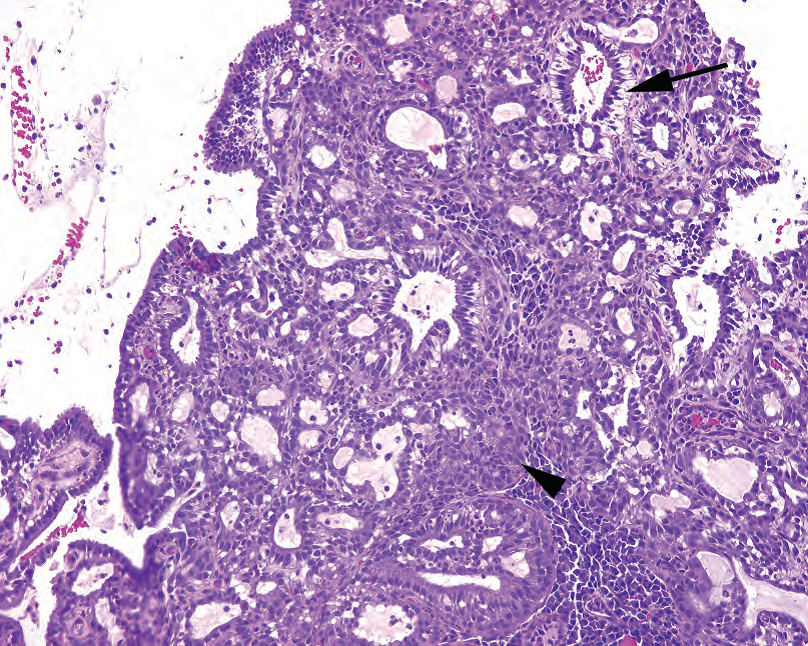
Figure 16.9. Microglandular hyperplasia. These endocervical glands show a very cellular proliferation composed of mucinous cells (arrow) and squamous metaplasia (arrowhead) and a cribriform pattern of lumens. This is benign.
图16.9 微腺体增生。这些宫颈腺体表现为一种非常富于细胞的增殖,由粘液细胞(箭)和鳞状化生(箭头)以及筛孔模式组成。这是良性的。
Endometriosis appears as dense blue palisaded columnar glands without mucus, surrounded by edematous endometrial-type stroma. The dark glands can be very eye catching and can even show mitoses, so recognizing the stroma is the key to making the diagnosis (Figure 16.10). The presence of extravasated red blood cells or hemosiderin is very helpful.
子宫内膜异位症表现为致密的、蓝色的、栅栏状排列的柱状腺体,无胞质粘液,周围为水肿的子宫内膜型间质。深染的腺体非常吸引眼球,甚至可以显示核分裂,因此识别间质是诊断的关键(图16.10)。存在红细胞外渗或含铁血黄素有助于诊断。
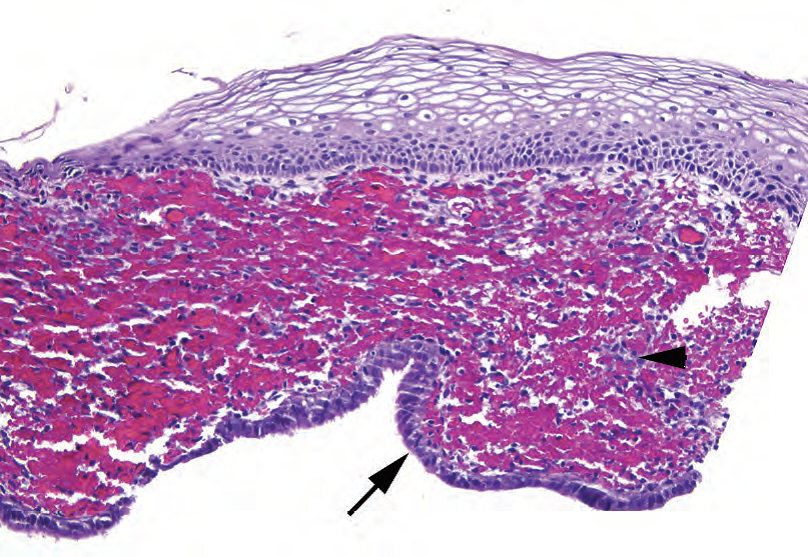
Figure 16.10. Endometriosis. This cervical biopsy specimen shows a squamous epithelium overlying stroma with hemorrhage. At the bottom of the fragment there is a dark cuboidal lining (arrow) resembling endometrial epithelium. The telltale endometrial stroma (arrowhead) is mostly obscured by blood.
图16.10 子宫内膜异位症。宫颈活检标本显示间质上方有鳞状上皮伴出血。在片段的底部被覆着类似子宫内膜上皮的深染立方形细胞(箭)。子宫内膜间质(箭头)大部分被血液遮盖。
腺体病变(Glandular Lesions)
Most pathologists do not use endocervical dysplasia as a diagnosis and only use the two ends of the spectrum, reactive atypia and AIS, for atypical noninvasive glandular lesions. Glands with AIS should stand out as being distinctly different from their benign neighbors (they look much darker). Recognizing these glands requires a conscious effort to look for them, however, because the eye tends to focus on the squamous epithelium, and AIS can be subtle at scanning magnification.
大多数病理学家不使用宫颈腺体异型增生作为诊断,只使用疾病谱系的两端,即,反应性非典型增生和原位腺癌(AIS),用于非典型非浸润性腺体病变。AIS腺体显得很突出,应该与良性腺体明显不同(明显地更加深染)。然而,识别这些异常腺体需要有意识地努力寻找,因为眼睛往往盯着鳞状上皮,而在扫描倍数时,AIS可能很微妙。
Features of AIS include the following:
AIS的特点包括:
Close clusters of dark glands may resemble intestinal crypts or a tubular adenoma (Figure 16.11).
紧密排列的成簇的深染腺体,可能类似结肠的隐窝或管状腺瘤(图16.11)。
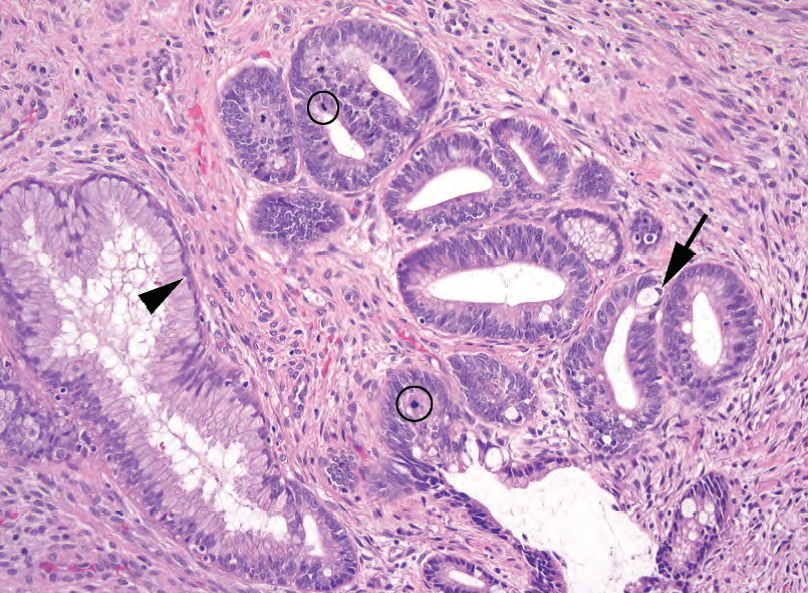
Figure 16.11. Adenocarcinoma in situ. This field shows some residual normal endocervical glands (arrowhead) adjacent to a very abnormal population with dark, elongated, crowded, and stratified nuclei representing adenocarcinoma in situ. Occasional intestinal-type goblet cells (arrow) and mitoses (circles) are present.
图16.11 原位腺癌。这个区域显示一些残留的正常宫颈腺体(箭头),邻近一群显著异常的腺体,后者呈现深染的、拉长的、拥挤的和复层化细胞核,代表原位腺癌。偶有肠型杯状细胞(箭)和核分裂(圆圈)。
Nuclei are tall and pseudostratified, enlarged, and hyperchromatic.
细胞核呈高柱状(译注,或笔杆状),假复层,增大,深染。
Nucleoli may be present.
核仁可能存在。
Luminal mitoses and apoptosis are common.
常见管腔面核分裂和凋亡。
Papillary or cribriform architecture may be present and, if confluent, should raise the possibility of stromal invasion.
可能存在乳头状或筛状结构,如果出现融合的筛状结构,应怀疑间质浸润的可能性。
Mucin may be present as scattered vacuoles or as discrete goblet cells (intestinal type).
可能存在胞质粘液,表现分散的胞质空泡或离散的杯状细胞(肠型)。
Ki67 staining is markedly elevated, and p16 staining should be diffusely positive (AIS is an HPV-associated lesion).
Ki67染色明显升高,p16染色应呈弥漫性阳性(AIS为HPV相关病变)。
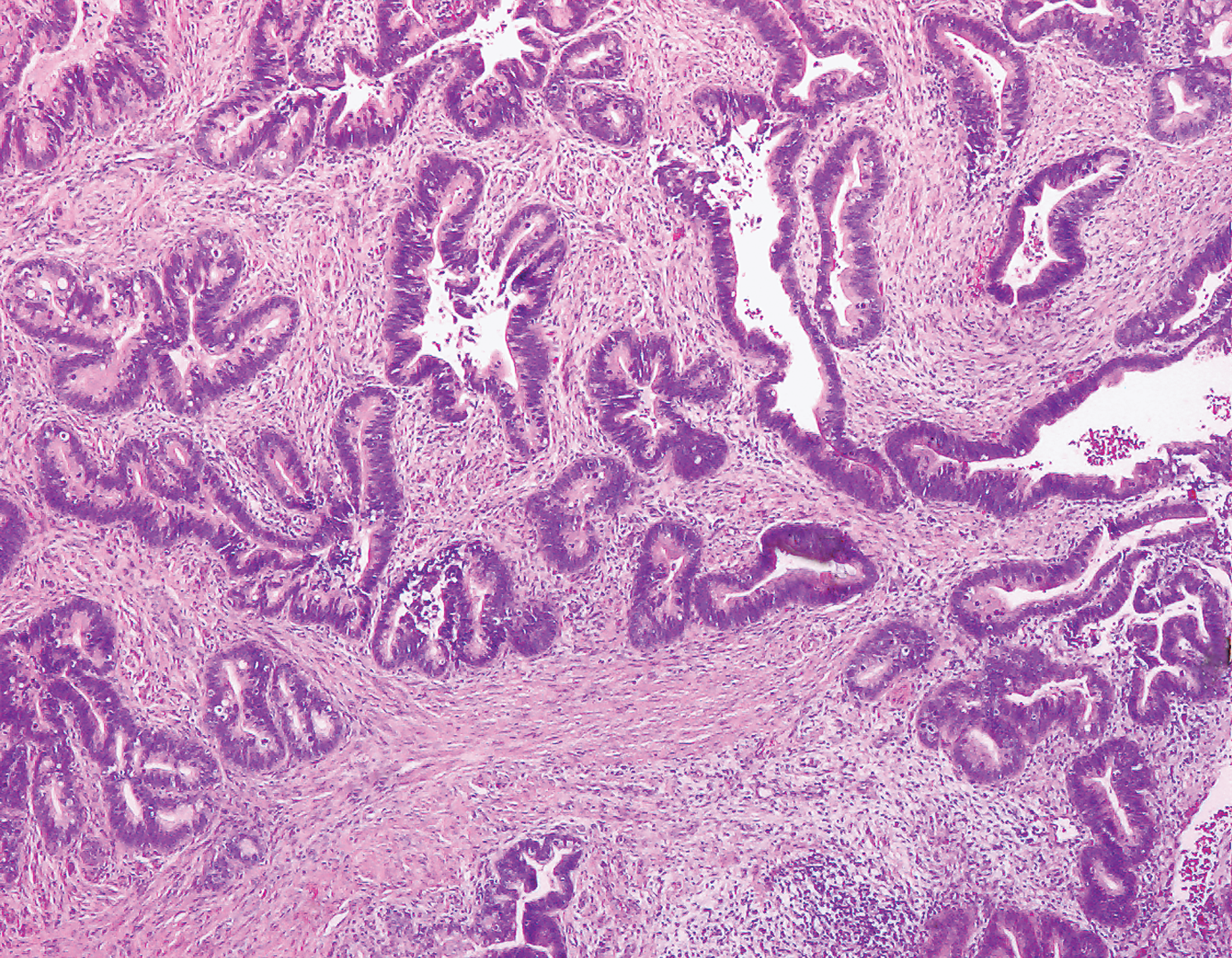
浸润性腺癌(Invasive Adenocarcinoma)
The most common variant of invasive adenocarcinoma is the endocervical type (“usual type”), which is an invasive form with the morphology seen in AIS. Features of invasion include the following:
浸润性腺癌的最常见变异型是宫颈内膜型(“普通型”),这是AIS所见形态的浸润性模式。浸润的特点包括:
Cell clusters diving off into the stroma, as with squamous cell carcinoma
细胞簇潜入间质,正如鳞状细胞癌那样
Desmoplastic response
促结缔组织增生反应
Glands that are significantly deeper into the stroma than the benign glands (on perpendicu-lar section)
腺体比良性腺体更深入间质(在垂直切片上观察)(译注:一般认为正常腺体深度不超过7mm)
Glands with AIS features that are too crowded, or back to back
具有AIS特征的腺体过于拥挤,或背靠背
Endocervical adenocarcinoma may be hard to distinguish from endometrial adenocarcinoma. However, the endocervical variety should be diffusely p16 positive, whereas the endometrial type is usually estrogen and progesterone positive. See images and test yourself on cervical lesions at http://screening.iarc.fr/atlashisto.php.
宫颈内膜腺癌可能很难与子宫内膜腺癌区分。然而,宫颈内膜腺癌应为p16弥漫阳性,而子宫内膜腺癌通常为雌激素受体(ER)和孕激素受体(PR)阳性。关于宫颈病变,可以网站查看图像并进行自测:http://screening.iarc.fr/atlashisto.php.
(译注:原文笔误,estrogen and progesterone应为estrogen and progesterone receptor)
(译注:补充宫颈内膜腺癌图片)
阴道和外阴上皮(Vaginal and Vulvar Epithelium)
Human papillomavirus can cause similar lesions in the vagina and vulva. As in the cervix, the lesions are grouped into low-grade and high-grade, corresponding to vaginal intraepithelial neoplasia grade 1 (VAIN1)/vulvar intraepithelial neoplasia grade 1 (VIN1) and VAIN2–3/VIN2–3. The clinical term bowenoid papulosis refers to VIN3, synonymous with carcinoma in situ (Figure 16.12). As in the cervix, these lesions can progress to invasive squamous cell carcinoma.
HPV可在阴道和外阴引起类似的病变。与宫颈一样,分为低度和高度病变,对应于阴道上皮内瘤变1级(VAIN1)/外阴上皮内瘤变1级(VIN1)和VAIN2-3/VIN2-3。临床术语鲍温样丘疹病是指VIN3,与原位癌为同义词(图16.12)。与宫颈一样,这些病变可进展为浸润性鳞状细胞癌。
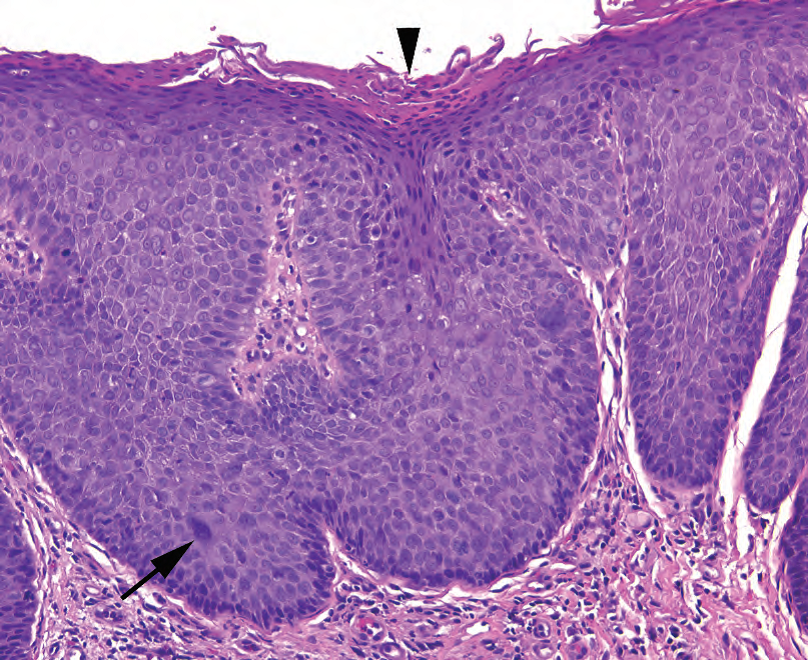
Figure 16.12. Vulvar intraepithelial neoplasia (VIN3). This biopsy specimen shows hyperkeratosis and parakeratosis (arrowhead) overlying a very blue squamous epithelium. Although the nuclear changes are not as obvious as in high-grade cervical lesions, there is loss of polarity and high nuclear/cytoplasmic ratios in the superficial epithelium. Occasional large atypical cells (arrow) are visible.
图16.12 外阴上皮内瘤变(VIN3)。活检标本显示覆盖在非常蓝染的鳞状上皮上方的角化过度和角化不全(箭头)。尽管核改变不如宫颈高度病变那样明显,但浅层上皮中细胞极性消失和核/质比增高。偶见大的非典型细胞(箭)。
乳头状病变(Papillary Lesions)
An exophytic viral lesion with LSIL-type changes is called a condyloma acuminatum. The LSIL features are somewhat subtler in a condyloma, and the nuclei may not be as obviously koilocytic. However, the presence of a verrucous (papillary, hyperkeratotic, and parakeratotic) lesion is virtually diagnostic of a condyloma (Figure 16.13). Non-HPV-related squamous papillomas also occur, usually in the vestibule, but without evidence of viral changes or hyperkeratosis. Finally, if the lesion is composed of more stroma than epithelium, it is most likely a fibroepithelial polyp (skin tag).
具有LSIL改变的外生病毒性病变称为尖锐湿疣。在尖锐湿疣中,LSIL的特征有点微妙,细胞核可能没有明显的挖空细胞改变。然而,出现疣状(乳头状、角化过度和角化不全)病变,实际上对湿疣具有诊断意义(图16.13)。非HPV相关的鳞状乳头状瘤也会发生,通常发生在前庭,但没有病毒改变或角化过度的证据。最后,如果病变的间质多于上皮,则很可能是纤维上皮性息肉(皮赘)。
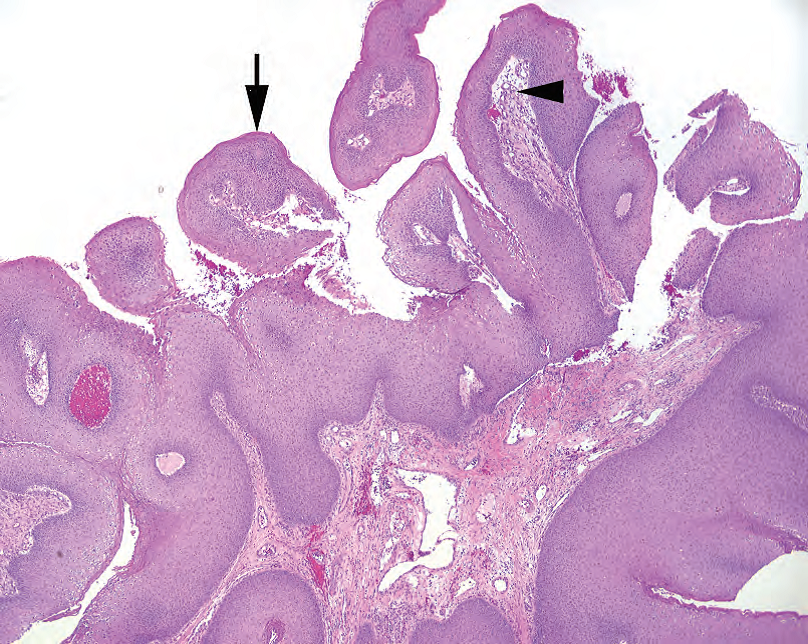
Figure 16.13. Condyloma. This exophytic lesion has prominent fibrovascular cores (arrowhead) underlying a thickened and hyperkeratotic squamous epithelium (arrow). Koilocytic or LSIL-type changes are not always obvious in condylomas.
图16.13 尖锐湿疣。这种外生性病变有明显的纤维血管轴心(箭头),位于增厚和角化过度的鳞状上皮下方(箭)。湿疣中挖空细胞或LSIL改变并不总是明显的。
炎症性皮肤病(Inflammatory Skin Conditions)
Lichen sclerosus appears as a flat, white, shiny patch clinically and in developed form looks like a bland pale swath of collagen (homogenous hyalinization) just beneath a thinned and flattened epidermis (Figure 16.14). Lichen simplex chronicus, on the other hand, is related to chronic spongiotic dermatitis and is characterized by epidermal thickening and hyperkeratosis over chronic inflammation in the dermis. It is a diagnosis of exclusion; you should first rule out fungal infection and squamous dysplasia.
硬化性苔藓在临床上表现为一种平坦的、白色的、有光泽的斑块,典型病变似乎在变薄、变平的表皮下方形成一条形态温和的、淡染的胶原带(均质透明变性)(图16.14)。慢性单纯性苔藓与慢性海绵状皮炎有关,其特征是表皮增厚和角化过度,而不是真皮慢性炎症。这是一种排除性诊断;你应该首先排除真菌感染和鳞状细胞异型增生。
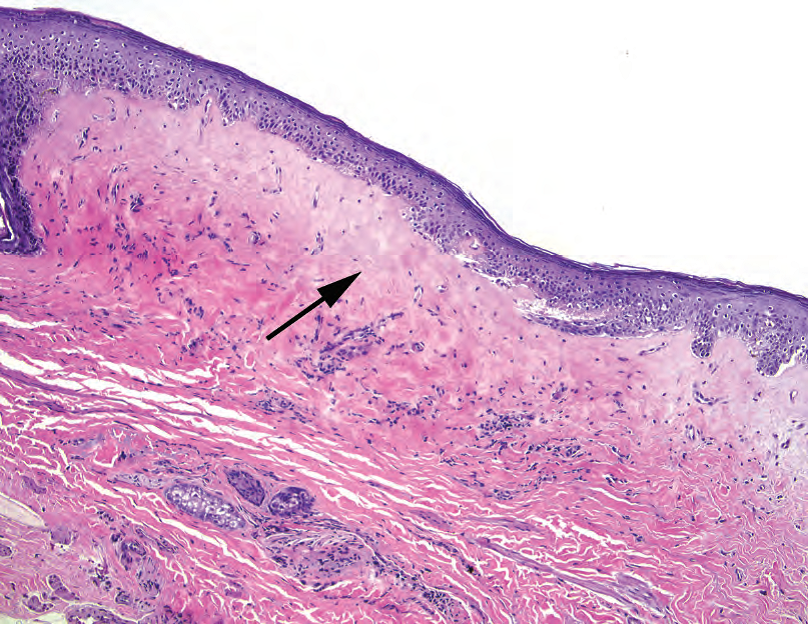
Figure 16.14. Lichen sclerosus. The epithelium is thin and atrophic, and the collagen underneath is pale, dense, and homogenized in texture (arrow). The dermal–epidermal junction is flattened, with an absence of rete.
图16.14 硬化性苔藓。上皮薄而萎缩,下面的胶原显得淡染、致密和质地均匀(箭)。真皮-表皮交界处变平,无上皮脚。
Paget’s disease, extramammary type, is not an inflammatory skin disorder but may be mistaken for one clinically. Unlike in the breast, it does not always indicate an underlying a denocarcinoma. However, in other respects it is analogous to mammary Paget’s, with large atypical carcinomatous cells percolating through a benign epidermis (Figure 16.15).
乳腺外型佩吉特病不是炎症性皮肤病,但临床可能误诊。与乳腺癌不同,它并不总是预示着下方存在腺癌。然而,它在其他方面类似于乳腺佩吉特病,典型表现为大的非典型细胞在良性表皮中浸润(图16.15)。
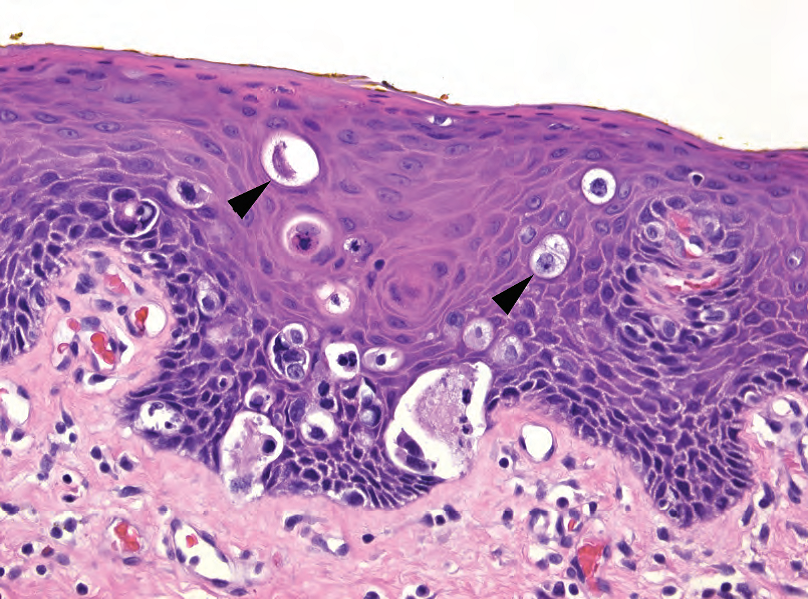
Figure 16.15. Paget’s disease. Several nonsquamous cells (arrowheads) are visible within the squamous epithelium.
图16.15 佩吉特病。鳞状上皮内可见数个非鳞状细胞(箭头)。
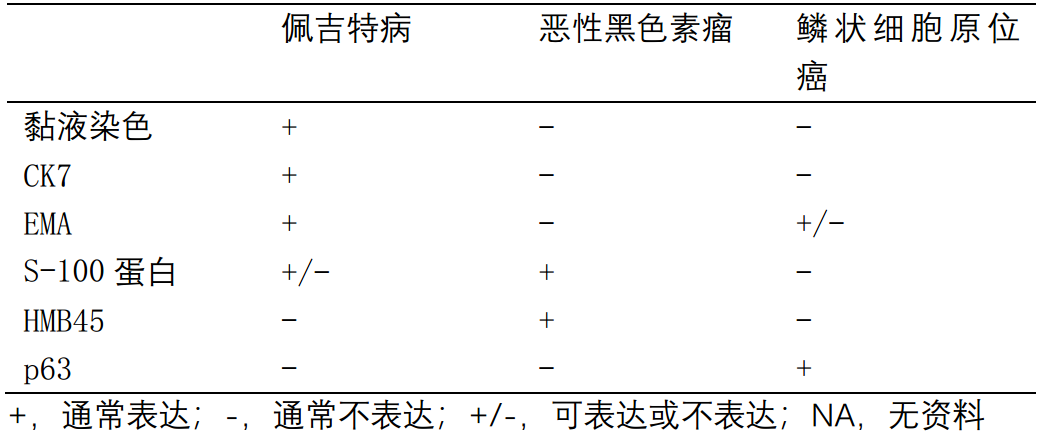
Melanoma, vulvar type, must always be in your differential diagnosis when you see pagetoidtype cells. A simple immunopanel will differentiate the two.
外阴型黑色素瘤:一旦看到佩吉特样细胞,你的鉴别诊断就一定要包括黑色素瘤。一个简单的免疫组化套餐就能区分两者。
(译注:补充一张表:佩吉特病及其相似病变的常用组织化学和免疫染色)
来源:
The Practice of Surgical Pathology:A Beginner’s Guide to the Diagnostic Process
外科病理学实践:诊断过程的初学者指南
Diana Weedman Molavi, MD, PhD
Sinai Hospital, Baltimore, Maryland
ISBN: 978-0-387-74485-8 e-ISBN: 978-0-387-74486-5
Library of Congress Control Number: 2007932936
© 2008 Springer Science+Business Media, LLC
仅供学习交流,不得用于其他任何途径。如有侵权,请联系删除。
本站欢迎原创文章投稿,来稿一经采用稿酬从优,投稿邮箱tougao@ipathology.com.cn
相关阅读
 数据加载中
数据加载中
我要评论

热点导读
-

淋巴瘤诊断中CD30检测那些事(五)
强子 华夏病理2022-06-02 -

【以例学病】肺结节状淋巴组织增生
华夏病理 华夏病理2022-05-31 -

这不是演习-一例穿刺活检的艰难诊断路
强子 华夏病理2022-05-26 -

黏液性血性胸水一例技术处理及诊断经验分享
华夏病理 华夏病理2022-05-25 -

中老年女性,怎么突发喘气困难?低度恶性纤维/肌纤维母细胞性肉瘤一例
华夏病理 华夏病理2022-05-07






共0条评论